Pediculosis corporis, or body lice infestation, is a parasitic condition caused by Pediculus humanus corporis, an obligate ectoparasite that lives in the seams of clothing and feeds on human blood. Though more prevalent in settings of poor hygiene and crowded living conditions, pediculosis corporis remains a significant concern for public health due to its potential to transmit severe infectious diseases.
Overview of Pediculus Humanus Corporis
Body lice are morphologically similar to head lice but differ in behavior and habitat. Unlike head lice, body lice dwell in clothing rather than on the skin and migrate to the host only to feed.
- Size: 2–4 mm, slightly larger than head lice
- Color: Grayish-white
- Mobility: Slower than head lice, yet capable of crawling
- Survival off host: Up to 10 days in clothing without feeding
Epidemiology and Risk Factors
Pediculosis corporis predominantly affects populations experiencing:
- Poor hygiene practices
- Lack of access to clean clothing or laundry facilities
- Homelessness, displacement, or natural disasters
- Crowded institutional environments (e.g., shelters, prisons, refugee camps)
Although rare in industrialized nations, outbreaks may still occur among vulnerable groups, warranting vigilant surveillance.
Lifecycle of Body Lice
The lifecycle of Pediculus humanus corporis involves three stages: egg (nit), nymph, and adult. Each stage is critical to the progression of infestation.
Clinical Manifestations of Pediculosis Corporis
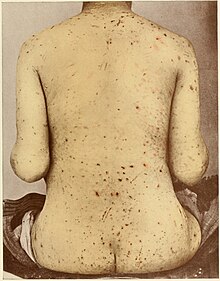
Body lice infestation may be asymptomatic initially but often progresses to include characteristic dermatologic and systemic signs.
Cutaneous Symptoms
- Intense pruritus, especially at night
- Erythematous macules and papules, typically on the trunk, shoulders, and thighs
- Excoriations and secondary bacterial infections from persistent scratching
- Post-inflammatory hyperpigmentation in chronic infestations
- Thickened, darkened skin (vagabond’s disease) due to prolonged exposure and scratching
Systemic Concerns
- Vector transmission of infectious diseases including:
- Rickettsia prowazekii (epidemic typhus)
- Borrelia recurrentis (relapsing fever)
- Bartonella quintana (trench fever)
Diagnostic Criteria for Body Lice Infestation
A diagnosis of pediculosis corporis is confirmed through direct identification of lice or nits within clothing, typically in seams or folds.
Key Diagnostic Methods
- Visual examination of clothing:
- Inspect seams, cuffs, waistbands, and underarm areas
- Presence of adult lice and nits confirms diagnosis
- Skin examination:
- Look for excoriated lesions and characteristic distribution of pruritic rash
- Dermoscopy (if available):
- Assists in identifying nits and lice fragments when visual confirmation is uncertain
Unlike scabies or head lice, body lice are rarely found directly on the skin for prolonged periods, making garment inspection essential.
Treatment and Management of Pediculosis Corporis
Eradication of body lice hinges on eliminating the lice’s environment rather than direct treatment of the skin.
Environmental Decontamination
- Immediate laundering of all clothing, bedding, and towels in hot water (≥130°F / 54°C)
- Machine drying on a high-heat cycle for at least 20 minutes
- Ironing seams of garments when laundering is unavailable
- Dry-cleaning or sealing clothes in plastic bags for 2 weeks to kill lice and nits
Personal Hygiene
- Regular bathing and changing into clean clothes
- Provision of clean garments in institutional settings
Pharmacologic Intervention (Rarely Required)
- Topical pediculicides (e.g., permethrin 5%) may be used on the body in resistant or complicated cases
- Ivermectin (oral) for severe or refractory infestations, especially in conjunction with decontamination efforts
Prevention of Body Lice Infestation
Institutional Protocols
- Routine screening in shelters, prisons, and refugee camps
- Access to laundry facilities, personal hygiene resources, and adequate clothing
- Education programs on lice identification and control measures
Public Health Interventions
- Rapid response to outbreaks with coordinated deinfestation procedures
- Surveillance for vector-borne infections associated with lice
- Hygiene kits distribution in disaster relief scenarios
Complications and Associated Infections
The primary public health significance of pediculosis corporis lies in its potential to act as a vector for severe infectious diseases.
| Disease | Causative Agent | Transmission | Symptoms |
|---|---|---|---|
| Epidemic Typhus | Rickettsia prowazekii | Louse feces enters skin abrasions | Fever, rash, delirium |
| Trench Fever | Bartonella quintana | Fecal contamination | Relapsing fever, bone pain |
| Relapsing Fever | Borrelia recurrentis | Louse crushing during scratching | Cyclic fevers, headache |
Prompt recognition of body lice infestations can prevent these complications and reduce mortality associated with vector-borne diseases.
Differentiating Pediculosis Corporis from Similar Conditions
| Condition | Key Features | Distinction |
|---|---|---|
| Scabies | Burrows, intense nocturnal itching, web spaces | Mite identified on skin, not clothing |
| Head Lice | Found on scalp and hair shafts | No involvement of clothing |
| Contact Dermatitis | Localized rash after allergen exposure | No lice or nits present |
| Eczema | Chronic dry, itchy patches | Symmetrical distribution, no nits |
Management in Vulnerable Populations
Pediculosis corporis disproportionately affects unsheltered individuals, those in conflict zones, and residents of long-term care facilities. Sustainable management requires:
- Multidisciplinary care teams
- Continuous provision of hygiene and laundry access
- Medical screening for associated infections
- Social support and housing interventions
Pediculosis corporis is more than a parasitic nuisance; it represents a marker of systemic social and public health gaps. Effective management relies on rapid identification, environmental decontamination, personal hygiene restoration, and prevention of transmission. Special emphasis must be placed on vulnerable populations through comprehensive hygiene access and healthcare services to mitigate recurrence and associated disease transmission.