Non-small cell lung cancer (NSCLC) encompasses a diverse group of lung malignancies, with metastatic cases requiring tailored treatment strategies. Among these, patients with PD-L1 positive, EGFR-negative, and ALK-negative metastatic NSCLC represent a distinct subgroup that benefits significantly from immune checkpoint blockade therapies. The absence of actionable mutations (EGFR, ALK) redirects the therapeutic focus toward PD-L1 expression as a predictive biomarker for immunotherapy responsiveness.
Understanding the Molecular Profile
The Significance of PD-L1 Expression
PD-L1 (programmed death-ligand 1) is a surface protein expressed by tumor cells and immune infiltrates. When bound to the PD-1 receptor on T cells, it inhibits T-cell activity, promoting immune escape. High PD-L1 expression (≥50% Tumor Proportion Score, TPS) is associated with increased likelihood of response to PD-1/PD-L1 inhibitors.
EGFR and ALK Wild-Type Status
Patients negative for epidermal growth factor receptor (EGFR) and anaplastic lymphoma kinase (ALK) mutations do not benefit from targeted tyrosine kinase inhibitors (TKIs), which are reserved for those with activating mutations. Their treatment path relies on immunotherapy or chemo-immunotherapy, determined by PD-L1 levels.
Diagnostic and Biomarker Testing in Advanced NSCLC
Accurate diagnosis and molecular profiling are essential before initiating treatment.
Essential Diagnostic Components:
- Histological Subtyping: Adenocarcinoma, squamous cell carcinoma, or large cell carcinoma.
- PD-L1 IHC Assays: 22C3 (Dako), 28-8 (Dako), SP263 (Ventana).
- Molecular Testing: EGFR, ALK, ROS1, BRAF, MET, RET, KRAS, and HER2.
Patients with PD-L1 TPS ≥ 1% and no detectable EGFR or ALK mutations qualify for checkpoint inhibition-based treatment strategies.
Frontline Treatment Strategies Based on PD-L1 Status
TPS ≥ 50%: Immunotherapy Monotherapy
In the absence of EGFR/ALK alterations, patients with high PD-L1 expression are candidates for monotherapy using PD-1/PD-L1 inhibitors:
- Pembrolizumab (Keytruda)
- Cemiplimab (Libtayo)
- Atezolizumab (Tecentriq) (for specific indications)
These therapies offer durable responses and reduced toxicity compared to chemotherapy.
Keynote-024 Findings (Pembrolizumab):
- Median overall survival (OS): 26.3 months vs. 13.4 months (chemo).
- Objective response rate (ORR): 44.8%.
- Reduced grade ≥3 toxicities.
TPS 1–49%: Immunotherapy with Chemotherapy
Patients with intermediate PD-L1 expression levels benefit most from combination therapy:
- Pembrolizumab + Platinum Doublet Chemotherapy
- Adenocarcinoma: Pemetrexed + Carboplatin/Cisplatin
- Squamous: Paclitaxel + Carboplatin
This combination enhances anti-tumor efficacy by inducing immunogenic cell death while promoting T-cell activation.
TPS < 1%: Chemo-ICI Combinations or Trials
Even without PD-L1 expression, select patients may benefit from combined modalities:
- Nivolumab + Ipilimumab + Chemotherapy
- Clinical trials involving emerging targets (e.g., LAG-3, TIGIT, STING agonists)
Treatment in this group requires careful consideration of performance status, comorbidities, and tumor burden.
Immune Checkpoint Inhibitors for EGFR-/ALK- NSCLC
| Drug | Mechanism | Indication | PD-L1 Threshold |
|---|---|---|---|
| Pembrolizumab | Anti–PD-1 | First-line monotherapy / combo with chemo | ≥1% / ≥50% |
| Atezolizumab | Anti–PD-L1 | Monotherapy or combo with bevacizumab/chemo | ≥50% (TC or IC) |
| Cemiplimab | Anti–PD-1 | Monotherapy for metastatic NSCLC | ≥50% |
| Nivolumab + Ipilimumab | PD-1 + CTLA-4 inhibition | First-line with chemo (CheckMate 9LA) | All-comers |
Resistance to Checkpoint Inhibition and Future Options
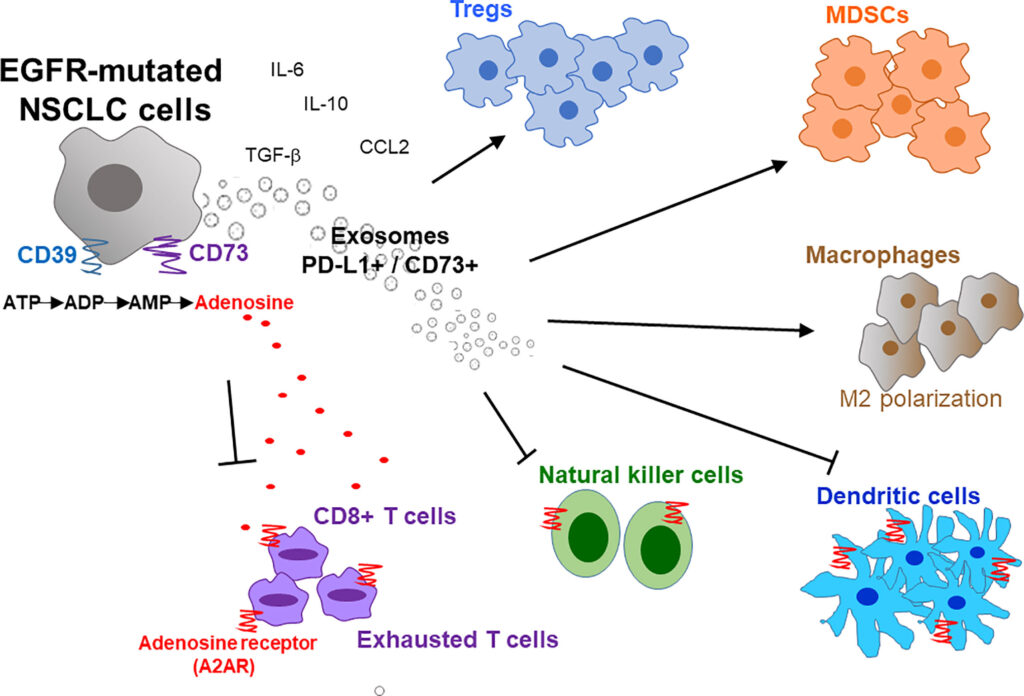
Mechanisms of Primary or Acquired Resistance
- Loss of antigen presentation via B2M mutations
- Infiltrative immunosuppressive macrophages and MDSCs
- Low tumor mutational burden (TMB)
- Alternate immune checkpoints activation (e.g., TIM-3, VISTA)
Investigational Strategies
- Bispecific antibodies targeting PD-1 and novel ligands
- Vaccines and neoantigen-specific T-cell therapies
- Adoptive cell transfer, including CAR-T for solid tumors
- Epigenetic modulators to reverse immune exclusion
Personalized Therapy Based on Comorbid Conditions
Key Factors in Treatment Decisions:
- Performance Status (ECOG): ≥2 may preclude aggressive regimens.
- Organ Function: Hepatic/renal insufficiency impacts chemotherapy eligibility.
- Brain Metastases: Favor agents with CNS penetration or upfront local therapy.
- Autoimmune Conditions: May contraindicate checkpoint blockade.
Prognosis and Long-Term Management
While metastatic NSCLC remains incurable, durable responses have been observed with immunotherapy, especially in PD-L1 high expressers. Median OS now exceeds 2–3 years in this subset. Continued monitoring with imaging and biomarkers (e.g., ctDNA) is essential to detect progression early.
The treatment landscape for PD-L1 positive, EGFR-negative, ALK-negative metastatic NSCLC has evolved to prioritize immune checkpoint blockade as a front-line approach. Biomarker-driven decisions, in conjunction with patient-specific factors, are vital to optimize outcomes. As new therapies and biomarkers emerge, therapeutic strategies continue to move toward precision immuno-oncology.