Pathological gastric acid hypersecretory condition refers to an abnormal increase in gastric acid production beyond physiological needs, often leading to severe gastrointestinal complications. This condition is primarily associated with diseases like Zollinger-Ellison syndrome, and is characterized by hypergastrinemia and excessive stimulation of parietal cells. Chronic acid overproduction disrupts mucosal integrity, increases ulcer formation risk, and may lead to gastrointestinal bleeding and malabsorption.
Physiological Regulation of Gastric Acid Secretion
Gastric acid secretion is tightly regulated by neural, hormonal, and paracrine signals. The three major stimulants include:
- Gastrin (hormone from G cells)
- Histamine (from enterochromaffin-like cells)
- Acetylcholine (via vagus nerve stimulation)
These act on parietal cells located in the gastric fundus, which secrete hydrochloric acid (HCl) through the H⁺/K⁺ ATPase proton pump.
Under pathological conditions, this regulatory mechanism becomes dysregulated, resulting in excessive acid secretion that the mucosal barrier cannot neutralize.
Causes of Gastric Acid Hypersecretion
Zollinger-Ellison Syndrome (ZES)
ZES is the prototypical hypersecretory disorder caused by gastrin-secreting neuroendocrine tumors (gastrinomas), typically located in the pancreas or duodenum. Gastrinomas stimulate parietal cells independently of normal feedback mechanisms.
Gastric Cell Hyperplasia
Hypertrophy or hyperplasia of parietal cells can independently lead to increased acid output. This may be idiopathic or secondary to prolonged gastrin stimulation.
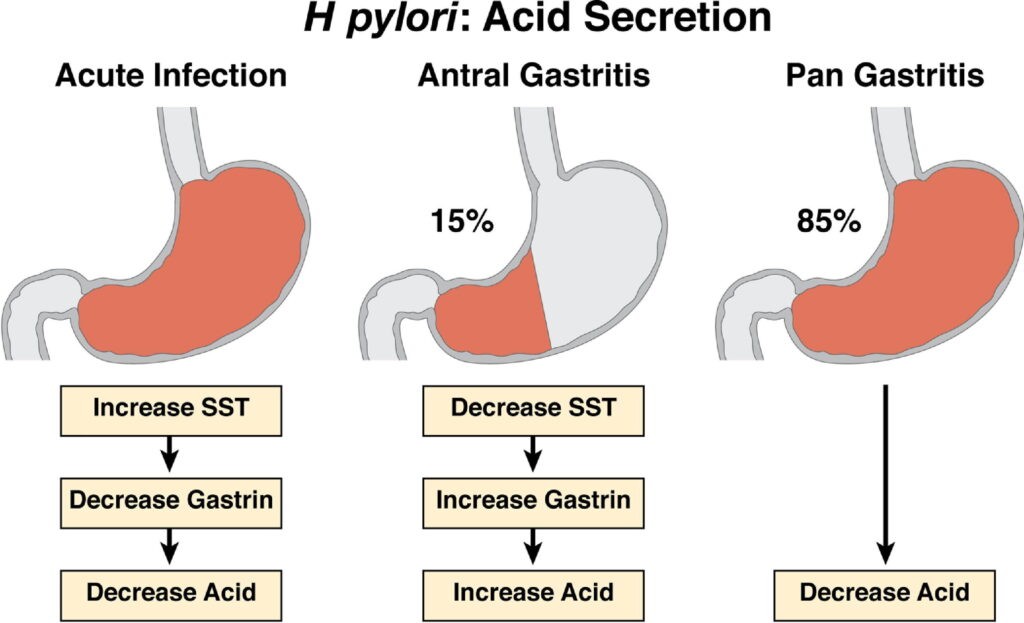
Helicobacter pylori Infection
H. pylori can elevate acid production in the early stages of infection by inhibiting somatostatin and allowing unchecked gastrin release.
Rebound Acid Hypersecretion
Abrupt withdrawal from proton pump inhibitors (PPIs) may induce transient acid hypersecretion due to compensatory parietal cell proliferation.
Clinical Manifestations of Hypersecretory Conditions
Gastrointestinal Symptoms
Patients typically present with:
- Refractory peptic ulcers (multiple, recurrent, or distal)
- Epigastric pain, particularly post-prandial
- Gastroesophageal reflux symptoms
- Diarrhea and steatorrhea in ZES due to enzyme inactivation
- Weight loss due to malabsorption or chronic discomfort
Complications
Uncontrolled acid hypersecretion can result in:
- Esophagitis
- Gastric metaplasia
- Bleeding ulcers
- Perforation
- Stricture formation
Diagnostic Approach to Gastric Acid Hypersecretion
Measurement of Gastric Acid Output
- Basal Acid Output (BAO): Normal < 10 mEq/hour; elevated in hypersecretory states.
- Maximal Acid Output (MAO): Measured after stimulation (e.g., pentagastrin).
Serum Gastrin Levels
Elevated fasting gastrin levels are a hallmark of ZES but must be interpreted with gastric pH data:
- Gastrin >1000 pg/mL + gastric pH < 2 is diagnostic of ZES.
- Moderate hypergastrinemia may require secretin stimulation testing.
Secretin Stimulation Test
A paradoxical rise in serum gastrin (>200 pg/mL) following secretin injection confirms gastrinoma.
Gastric pH Monitoring
Persistent pH < 2 under fasting conditions indicates acid hypersecretion and supports gastrin-mediated etiology.
Imaging and Tumor Localization
- Endoscopic ultrasound (EUS)
- Somatostatin receptor scintigraphy (Octreoscan)
- CT/MRI for metastases
- Selective arterial secretagogue injection (SASI)
Pathophysiology of Zollinger-Ellison Syndrome
In ZES, gastrinomas stimulate continuous gastric acid secretion. Unlike physiologic gastrin release, this is not downregulated by luminal acidity. Elevated acid loads cause mucosal injury and hinder pancreatic enzyme activity in the small intestine.
Gastrinomas may occur sporadically or in association with Multiple Endocrine Neoplasia type 1 (MEN1).
Differentiating Hypergastrinemia
| Condition | Gastrin Level | Gastric pH | Acid Output |
|---|---|---|---|
| ZES | High (>1000) | Low (<2) | Increased |
| Atrophic Gastritis | High | High (>4) | Low |
| PPI Therapy | High | High | Low |
Accurate distinction is essential for appropriate management and to avoid misdiagnosis.
Treatment of Gastric Acid Hypersecretory Conditions
Medical Therapy
- Proton Pump Inhibitors (PPIs): Mainstay therapy to suppress acid production. High-dose omeprazole or esomeprazole are used in ZES.
- Histamine H2 Receptor Antagonists: Less potent, used adjunctively or if PPIs are contraindicated.
- Somatostatin Analogues (e.g., Octreotide): Control hormone secretion in gastrinoma.
Surgical Management
- Curative Resection: Possible in localized gastrinomas without metastasis.
- Debulking Surgery: In metastatic cases to reduce tumor burden.
- Total Gastrectomy: Rarely indicated in refractory acid hypersecretion despite medical therapy.
Management of Underlying Causes
- H. pylori Eradication where applicable
- MEN1 Screening in familial cases of ZES
- Nutritional Support for patients with malabsorption
Prognosis and Follow-Up
The prognosis varies based on the underlying cause:
- Sporadic gastrinomas have better outcomes if surgically resectable.
- Metastatic or MEN1-associated tumors require lifelong PPI therapy and periodic imaging.
- Gastric complications like bleeding ulcers or strictures may need endoscopic or surgical intervention.
Routine monitoring of serum gastrin, gastric pH, and tumor imaging is essential to assess control and recurrence.
Pathological gastric acid hypersecretory conditions represent a complex spectrum of diseases primarily driven by excessive gastrin activity or parietal cell dysfunction. Accurate diagnosis through acid output studies, hormonal assays, and imaging is crucial to differentiate between causes such as Zollinger-Ellison syndrome and PPI-induced hypergastrinemia. Timely medical management with proton pump inhibitors and appropriate surgical intervention, when feasible, significantly improve patient outcomes. Lifelong monitoring remains a critical component of care to prevent relapse and manage complications.