Partial epilepsy, also referred to as focal epilepsy, originates in a specific region of the cerebral cortex. Seizures can remain localized or evolve into generalized seizures. When first-line antiepileptic drugs (AEDs) fail to provide sufficient control, adjunctive treatments—used in combination with baseline therapy—offer critical support in reducing seizure frequency and improving quality of life.
Adjunctive therapy for partial epilepsy aims to optimize seizure control while minimizing adverse effects. These strategies include the use of additional antiepileptic medications, neuromodulation techniques, and in selected cases, surgical interventions.
Pharmacological Adjunctive Therapies: Antiepileptic Drug Combinations
Indications for Adjunctive AED Therapy
Adjunctive therapy is generally indicated in:
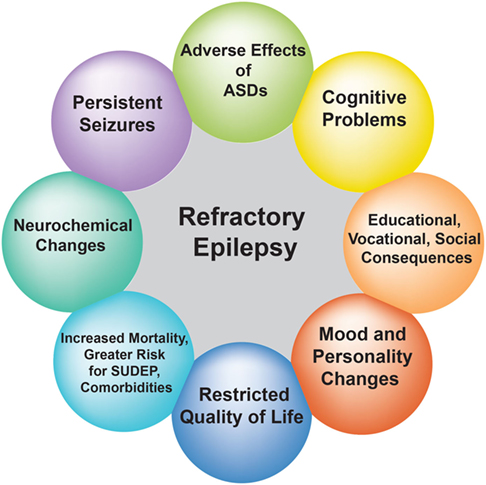
- Refractory partial epilepsy where monotherapy is ineffective
- Progressive or worsening seizure patterns
- Patients intolerant to higher doses of a single AED
Common Adjunctive Antiepileptic Medications
Several second- and third-generation AEDs have shown efficacy in partial epilepsy as add-on therapy:
Levetiracetam (LEV)
- Mechanism: SV2A receptor modulation
- Advantages: Well-tolerated, minimal interactions
- Typical Use: Broad-spectrum adjunct for adults and children
Lacosamide (LCM)
- Mechanism: Enhances slow inactivation of sodium channels
- Benefits: Effective in drug-resistant partial seizures
- Dosing: Initiated at 50 mg BID, titrated gradually
Brivaracetam (BRV)
- Mechanism: High-affinity SV2A binding
- Compared to LEV: Faster brain penetration, fewer psychiatric side effects
Perampanel (PER)
- Mechanism: AMPA receptor antagonist
- Indicated for focal and generalized seizures
- Caution: Associated with behavioral adverse effects
Topiramate (TPM) and Zonisamide (ZNS)
- Mechanisms: Broad spectrum—blocks sodium channels, enhances GABA activity
- Often used in combination with sodium channel inhibitors
Eslicarbazepine Acetate (ESL)
- Mechanism: Voltage-gated sodium channel blocker
- Lower risk of hyponatremia than carbamazepine
Non-Pharmacological Adjunctive Treatments for Partial Epilepsy
Vagus Nerve Stimulation (VNS)
A neurostimulation approach using an implanted device that intermittently stimulates the left vagus nerve.
- Mechanism: Alters neurotransmitter release and cortical excitability
- Indications: Drug-resistant focal epilepsy
- Outcomes: 30–50% seizure reduction in many patients
Responsive Neurostimulation (RNS)
An implantable device detects seizure activity in real-time and delivers direct electrical stimulation to the seizure focus.
- Customized Therapy: Tailored to patient-specific seizure patterns
- Effective in: Unilateral or bilateral seizure foci
Deep Brain Stimulation (DBS)
Primarily targets the anterior nucleus of the thalamus for seizure modulation.
- Utility: For patients with multiple foci or generalized spread
- Approved For: Refractory focal seizures in adults
Dietary and Lifestyle Interventions as Adjuncts
Ketogenic and Modified Atkins Diets
High-fat, low-carbohydrate diets that induce ketosis, which stabilizes neuronal membranes and reduces seizure activity.
- Ketogenic Diet: Best for children with refractory epilepsy
- Modified Atkins: Easier compliance for adolescents and adults
Sleep and Stress Management
- Importance: Poor sleep and high stress can precipitate seizures
- Adjunct Approaches: Cognitive behavioral therapy (CBT), mindfulness, structured routines
Clinical Considerations in Adjunct Therapy Selection
Factors Influencing Adjunct AED Choice
- Seizure Type and Frequency
- Patient Age and Comorbidities
- Drug Interaction Profile
- Tolerability and Past Response
Monitoring and Adjustment
- Regular EEGs and Seizure Diaries
- Blood Drug Levels When Necessary
- Renal and Hepatic Function Monitoring
When to Consider Surgery
- Patients failing two or more AEDs with clearly localized seizure focus
- Evaluation through video-EEG monitoring, MRI, and functional imaging
Efficacy of Adjunctive Treatments: Evidence and Outcomes
Clinical Trial Highlights
- LEV and BRV: Demonstrated >50% responder rates in >30% of subjects in Phase III trials
- VNS: Long-term studies show consistent seizure reduction over years
- RNS: Offers personalized treatment, with sustained seizure control and cognitive stability
Real-World Evidence
- Polytherapy often increases seizure-free intervals
- Early adjunct introduction in drug-resistant cases correlates with better prognosis
Adjunctive therapy in partial epilepsy is a dynamic and evolving field. For individuals who do not achieve seizure control through monotherapy, adjunctive antiepileptic drugs, neuromodulation techniques, dietary modifications, and, when indicated, surgical interventions collectively offer a comprehensive approach. A personalized treatment plan, guided by patient-specific variables and clinical data, maximizes efficacy while minimizing adverse effects. Clinicians must remain vigilant in monitoring treatment response and be prepared to adjust strategies based on emerging evidence and individual outcomes.