Partial central diabetes insipidus is a subtype of central diabetes insipidus characterized by incomplete deficiency of arginine vasopressin (AVP), also known as antidiuretic hormone (ADH). Unlike complete CDI, where AVP secretion is nearly absent, the partial form involves a measurable but insufficient level of AVP production, leading to impaired water reabsorption and mild to moderate polyuria and polydipsia.
Pathophysiology of AVP Deficiency
The hypothalamic-neurohypophyseal system is responsible for synthesizing and releasing AVP. Partial central DI arises from dysfunction within this axis due to partial neuronal loss or reduced AVP release capacity. The hormone acts on renal collecting ducts via V2 receptors, promoting water reabsorption. In partial CDI, this process is suboptimal, resulting in an inability to concentrate urine adequately under normal hydration or dehydration conditions.
Etiology: Causes and Risk Factors of Partial Central Diabetes Insipidus
Partial CDI may result from a range of congenital and acquired conditions. In some cases, the AVP deficiency is idiopathic, while in others it may stem from identifiable neurological or systemic events.
Congenital Causes
- Genetic mutations in AVP gene
- Developmental hypothalamic or pituitary malformations
Acquired Causes
- Trauma: Head injury affecting the hypothalamic-pituitary axis
- Neurosurgery: Especially involving craniopharyngiomas or pituitary tumors
- Infection and Inflammation: Tuberculosis, meningitis, encephalitis
- Neoplastic Conditions: Germinomas, metastatic cancers
- Idiopathic: No clear cause in up to 30% of cases
Clinical Features and Symptoms
Common Presentations
- Polyuria: Typically 3–7 liters/day (less than complete CDI)
- Polydipsia: Strong thirst for cold water
- Nocturia: Frequent urination disrupting sleep
- Normal Serum Sodium: Due to preserved partial AVP response
Differential Symptoms
- Less pronounced dehydration and hypernatremia compared to complete CDI
- Some capacity to concentrate urine during water deprivation
Diagnostic Approach to Partial Central Diabetes Insipidus
A thorough diagnostic workup is essential to distinguish partial CDI from complete CDI, nephrogenic diabetes insipidus (NDI), and primary polydipsia.
Stepwise Diagnostic Process
- 24-Hour Urine Volume and Osmolality
- Polyuria defined as >2.5 L/day with urine osmolality <300 mOsm/kg
- Water Deprivation Test
- Gradual fluid restriction under supervision
- In partial CDI, urine osmolality increases modestly
- Differentiates from complete CDI (no change) and primary polydipsia (significant increase)
- Desmopressin (DDAVP) Response Test
- Administered after water deprivation
- Partial CDI shows a marked rise in urine osmolality (>50%) post-DDAVP
- Serum Sodium and Plasma Osmolality
- Often normal but may reveal mild hypernatremia in undiagnosed cases
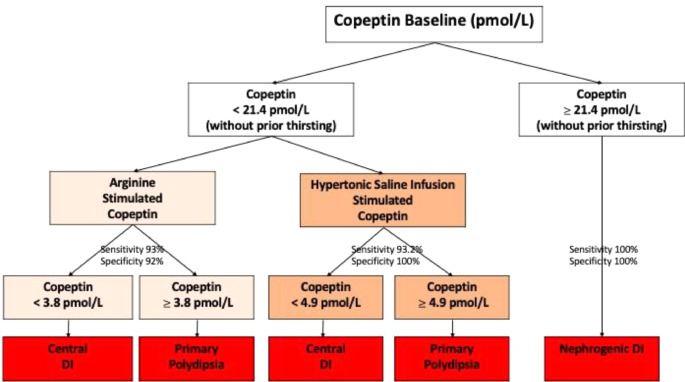
- Plasma AVP or Copeptin Levels
- Copeptin, a more stable AVP surrogate, helps differentiate CDI from NDI
Imaging Evaluation
Magnetic Resonance Imaging (MRI)
MRI of the brain and pituitary is critical in identifying structural causes:
- Loss of Posterior Pituitary Bright Spot: Indicative of AVP deficiency
- Hypothalamic or Pituitary Lesions: Tumors, inflammation, cysts
- Empty Sella Syndrome: Sometimes linked with CDI
Treatment and Long-Term Management of Partial CDI
Desmopressin (DDAVP) Therapy
Desmopressin is the synthetic analog of AVP and the mainstay treatment. In partial CDI, lower or less frequent doses are typically effective.
Routes of Administration
- Oral tablets
- Intranasal spray
- Subcutaneous or intravenous injection
Dosing Considerations
- Tailored to avoid hyponatremia due to water retention
- Dose titration based on urine output, body weight, and serum sodium
Lifestyle and Fluid Management
- Encourage fluid intake in proportion to urinary loss
- Monitor body weight and signs of overhydration or dehydration
- Educate on adjusting fluid intake during illness or heat exposure
Prognosis and Complications
Prognosis
With appropriate treatment, patients with partial CDI can lead normal lives with minimal disruption. Prognosis largely depends on underlying cause and adherence to therapy.
Potential Complications
- Hyponatremia: Overcorrection with desmopressin
- Dehydration: Missed doses or restricted access to water
- Growth and Developmental Delays: In children if undiagnosed
- Psychological Stress: Due to frequent urination and thirst
Comparison: Partial vs. Complete Central DI vs. Nephrogenic DI
| Feature | Partial CDI | Complete CDI | Nephrogenic DI |
|---|---|---|---|
| AVP Production | Reduced | Absent | Normal |
| Kidney Response to AVP | Normal | Normal | Impaired |
| Urine Osmolality (baseline) | Low (moderately) | Very low | Very low |
| Response to DDAVP | Moderate increase | Significant increase | No increase |
| Serum Sodium | Normal or mildly high | High | High |
Partial central diabetes insipidus, while less severe than its complete counterpart, demands precise diagnosis and careful long-term management to prevent complications and preserve quality of life. By combining clinical acumen with diagnostic testing—including water deprivation and DDAVP challenge—clinicians can distinguish partial CDI from other polyuric syndromes. With targeted desmopressin therapy and structured follow-up, patients can achieve effective symptom control and maintain electrolyte balance.