Paroxysmal atrial flutter is a type of supraventricular tachycardia marked by intermittent episodes of rapid and regular atrial contractions. Unlike persistent or chronic atrial flutter, paroxysmal forms are self-limited, lasting for minutes to several hours, and often terminate spontaneously. This condition poses significant clinical relevance due to its potential progression to atrial fibrillation and increased thromboembolic risk.
Mechanism and Pathophysiology of Paroxysmal Atrial Flutter
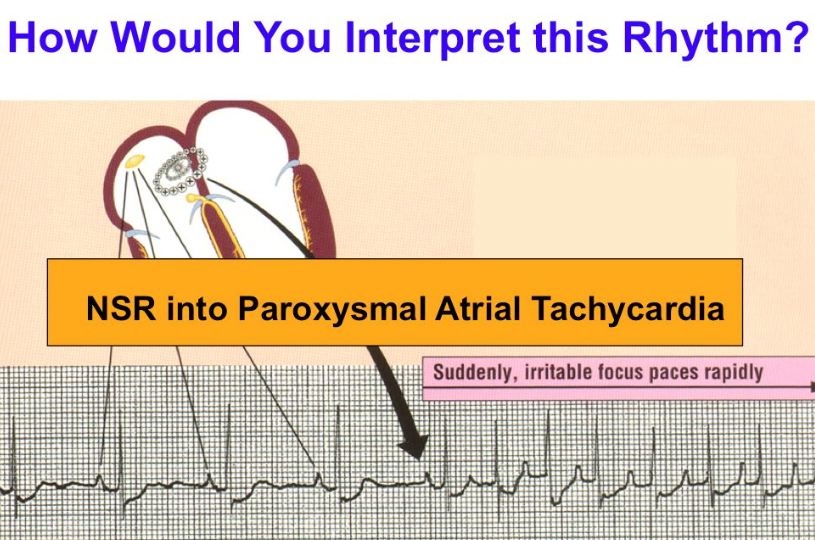
Atrial flutter originates from a macro-reentrant circuit, usually in the right atrium. The most common form, typical atrial flutter, involves a counterclockwise loop around the tricuspid annulus. In paroxysmal presentations, this reentry mechanism is triggered by premature atrial contractions, often in structurally remodeled atria.
Causes and Risk Factors Associated with Paroxysmal Atrial Flutter
Primary Causes
- Post-cardiac surgery or catheter ablation
- Structural heart disease
- Valvular heart disorders
- Hypertension
- Coronary artery disease
- Congenital heart defects
Contributing Risk Factors
| Risk Factor Category | Specific Examples |
|---|---|
| Lifestyle-Related | Alcohol, stimulant use, excessive caffeine |
| Systemic Conditions | Hyperthyroidism, sleep apnea, diabetes |
| Age and Gender | Increased risk in older males |
| Medication Effects | Digoxin toxicity, antiarrhythmic withdrawal |
Clinical Features and Symptoms of Paroxysmal Atrial Flutter
Symptoms can be sudden and distressing, particularly in individuals with compromised cardiac function. Symptom intensity varies depending on ventricular response rate and underlying cardiac status.
Common Symptoms
- Palpitations or fluttering sensation in the chest
- Sudden onset of rapid heart rate (100–150 bpm)
- Lightheadedness or dizziness
- Fatigue or decreased exercise tolerance
- Shortness of breath
- Mild chest discomfort or pressure
- Anxiety during episodes
In some cases, paroxysmal atrial flutter may be asymptomatic and detected incidentally on ECG or Holter monitoring.
Diagnostic Approach for Paroxysmal Atrial Flutter
Accurate and timely diagnosis is vital to managing paroxysmal atrial flutter effectively and preventing complications such as stroke or tachycardia-induced cardiomyopathy.
Diagnostic Methods
- Electrocardiogram (ECG): Identifies the classic “sawtooth” flutter waves, particularly in leads II, III, and aVF
- Holter Monitor: Monitors intermittent episodes over 24–72 hours
- Event Monitor or Loop Recorder: Captures infrequent episodes over longer periods
- Echocardiography: Evaluates atrial size, valve status, and left atrial thrombus
- Electrophysiological Study (EPS): Maps reentrant circuits, especially prior to ablation
Classification of Atrial Flutter
| Type | Characteristics |
|---|---|
| Typical Atrial Flutter | Counterclockwise macro-reentrant circuit in the right atrium |
| Atypical Atrial Flutter | Non-cavotricuspid circuits, post-surgical or scar-based |
| Paroxysmal | Episodes terminate spontaneously, <7 days |
| Persistent | Lasts >7 days or requires intervention |
| Permanent | Persistent and not amenable to rhythm correction |
Complications of Untreated Paroxysmal Atrial Flutter
- Thromboembolism and Stroke: Due to ineffective atrial contraction and blood stasis
- Heart Failure: From sustained rapid ventricular rate
- Progression to Atrial Fibrillation: Shared pathophysiological mechanisms
- Tachycardia-Induced Cardiomyopathy: In long-standing untreated episodes
Treatment and Management of Paroxysmal Atrial Flutter
Management aims to control rhythm, prevent recurrence, and reduce thromboembolic risk.
Acute Episode Management
- Rate Control: Beta-blockers, calcium channel blockers, or digoxin
- Rhythm Conversion:
- Pharmacological: Ibutilide, flecainide (under monitoring)
- Electrical Cardioversion: Preferred if hemodynamically unstable
Long-Term Strategy
- Catheter Ablation: First-line therapy for typical flutter due to high success rates (>90%)
- Antiarrhythmic Drugs: Amiodarone, sotalol, or class IC agents as needed
- Anticoagulation: Based on CHA₂DS₂-VASc score, even for brief episodes
- Lifestyle Modifications: Addressing triggers such as sleep apnea, alcohol, or weight gain
Prevention and Prognosis
Early diagnosis and definitive therapy such as catheter ablation significantly reduce recurrence rates and improve quality of life. Prognosis is favorable when treated promptly and complications are avoided.
Summary Table: Key Differences Between Paroxysmal Flutter and Fibrillation
| Feature | Paroxysmal Atrial Flutter | Paroxysmal Atrial Fibrillation |
|---|---|---|
| Atrial Rhythm | Regular | Irregular |
| Atrial Rate | 240–340 bpm | 350–600 bpm |
| ECG Appearance | Sawtooth waves | No discrete P waves |
| Circuit Type | Macro-reentrant | Multiple micro-reentrant foci |
| Ablation Success | High | Moderate |
Paroxysmal atrial flutter, though often transient, requires comprehensive evaluation and prompt management due to its potential to cause severe cardiovascular complications. With accurate diagnosis, targeted treatment, and preventative strategies, patients can achieve optimal outcomes and reduce the risk of long-term morbidity. Catheter ablation remains the cornerstone of treatment in eligible individuals, offering a durable cure and improved quality of life.