Parasitic infections remain a significant global health concern, especially in regions with limited access to clean water, sanitation, and healthcare. A parasitic infection occurs when a parasite—an organism that lives on or inside a host—invades the human body and disrupts normal physiological functions. These organisms derive nutrients at the host’s expense, often leading to severe illness, nutritional deficiencies, and chronic complications if left untreated.
Parasitic diseases are caused by three main types of organisms:
- Protozoa: Single-celled organisms that multiply in humans
- Helminths: Multicellular parasitic worms
- Ectoparasites: Organisms like lice and mites that live on the skin
Major Types of Human Parasitic Infections
1. Protozoan Infections
Protozoa are microscopic organisms transmitted primarily through contaminated water or food. Notable examples include:
- Giardiasis (caused by Giardia lamblia)
- Amebiasis (caused by Entamoeba histolytica)
- Malaria (caused by Plasmodium species)
- Toxoplasmosis (caused by Toxoplasma gondii)
These infections can lead to severe diarrhea, fatigue, and organ damage.
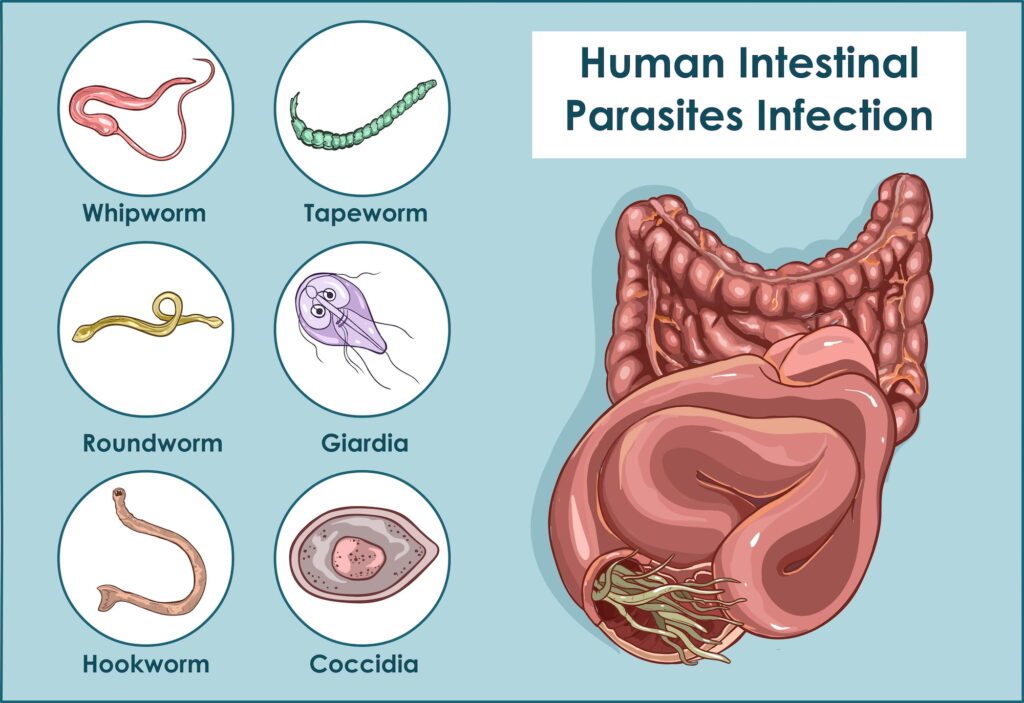
2. Helminthic Infections
Helminths are parasitic worms that inhabit the intestines or tissues. Categories include:
- Nematodes (roundworms): e.g., Ascaris lumbricoides, Enterobius vermicularis
- Trematodes (flukes): e.g., Schistosoma species
- Cestodes (tapeworms): e.g., Taenia saginata, Echinococcus granulosus
Symptoms often include abdominal pain, nutritional deficiency, and anemia.
3. Ectoparasitic Infestations
These parasites live externally on the body and include:
- Lice (head, body, and pubic)
- Scabies (caused by Sarcoptes scabiei)
- Ticks and fleas, which can also transmit other diseases
They commonly result in itching, skin irritation, and secondary infections.
Common Symptoms of Parasitic Infections
Parasitic symptoms vary depending on the species and site of infection. General manifestations include:
- Persistent diarrhea or constipation
- Abdominal cramping and bloating
- Unexplained weight loss
- Fatigue and weakness
- Itching or skin rash
- Fever and night sweats
- Anemia and malnutrition
In chronic cases, neurological symptoms, organ damage, or immunological responses may develop.
Routes of Transmission
Understanding transmission is critical to prevention. Common routes include:
- Fecal-oral: Contaminated food and water (e.g., giardiasis)
- Vector-borne: Insect bites, such as mosquitoes (e.g., malaria)
- Skin penetration: From contaminated soil or water (e.g., schistosomiasis)
- Direct contact: Human-to-human transmission via skin or bodily fluids (e.g., scabies)
- Zoonotic: From infected animals (e.g., toxoplasmosis)
Diagnostic Techniques for Accurate Detection
Timely diagnosis is essential to effective treatment. Key diagnostic tools include:
Stool Examination
- Detects eggs, cysts, and larvae
- Requires multiple samples over time
- Particularly useful for intestinal parasites
Blood Tests
- Detect antibodies or parasite DNA
- Used for malaria, toxoplasmosis, and filariasis
Imaging
- CT, MRI, or ultrasound can reveal cysts, abscesses, or organ involvement
- Commonly used in echinococcosis or neurocysticercosis
Skin Scraping or Biopsy
- Confirms ectoparasitic infestations such as scabies
- Identifies tissue-dwelling parasites
Treatment of Parasitic Infections
Treatment depends on the type of parasite and severity of the infection.
Antiparasitic Medications
- Metronidazole: For protozoa like Giardia and Entamoeba
- Albendazole and Mebendazole: Broad-spectrum anti-helminthic agents
- Praziquantel: Effective against flukes and tapeworms
- Ivermectin: For filarial infections and ectoparasites
- Chloroquine and Artemisinin: Used for malaria treatment
Supportive Therapy
- Rehydration therapy for fluid loss
- Nutritional support to counter deficiencies
- Iron and folic acid supplementation for anemic patients
Preventive Measures and Public Health Strategies
Hygiene and Sanitation
- Use clean, filtered water for drinking and cooking
- Wash hands thoroughly after using the restroom or handling raw food
- Cook meat and fish thoroughly to kill larvae or eggs
- Avoid walking barefoot in contaminated areas
Vector Control
- Use mosquito nets and repellents in endemic regions
- Control of animal reservoirs through veterinary surveillance
- Environmental sanitation to reduce breeding sites
Health Education
- Educating communities about the dangers of parasitic infections
- Promoting deworming programs in schools and rural populations
- Raising awareness of zoonotic risks from domestic animals
Parasitic Infections in Immunocompromised Individuals
People with weakened immune systems—such as those with HIV/AIDS or undergoing chemotherapy—are at higher risk of severe parasitic infections. Opportunistic infections like cryptosporidiosis, toxoplasmosis, and strongyloidiasis can lead to life-threatening complications. Prophylactic medication and regular monitoring are essential in these populations.
Emerging Parasitic Threats and Drug Resistance
Resistance to antiparasitic drugs is rising, particularly in malaria-endemic zones. The emergence of artemisinin-resistant Plasmodium falciparum strains in Southeast Asia underscores the urgent need for new treatment protocols and surveillance mechanisms. Additionally, climate change and global travel are expanding the range of vector-borne parasites to non-endemic regions.
Frequently Asked Questions:
What causes a parasitic infection?
Parasitic infections are caused by protozoa, helminths, or ectoparasites entering the human body through contaminated food, water, vectors, or direct contact.
How can I tell if I have a parasite?
Symptoms such as prolonged digestive issues, fatigue, itching, or visible worms in stool may indicate a parasitic infection. Seek medical testing for confirmation.
Are parasitic infections contagious?
Some parasitic infections, like giardiasis or scabies, can spread between humans via contact or shared resources. Proper hygiene reduces this risk.
Can parasitic infections be cured?
Yes. Most parasitic infections are treatable with specific antiparasitic medications. Early detection ensures faster recovery and fewer complications.
How can I prevent parasitic infections while traveling?
Drink only bottled or purified water, avoid raw or undercooked food, practice good hygiene, and use insect repellent in high-risk areas.
Parasitic infections remain a pervasive threat to public health, particularly in under-resourced regions. Comprehensive understanding, early diagnosis, and targeted treatment are vital to controlling their spread. Preventive strategies—including hygiene, education, vector control, and responsible medication use—must be integrated into public health policy and individual practice to effectively combat parasitic diseases and their long-term consequences.