Paralytic ileus is a functional impairment of intestinal motility without a mechanical obstruction, frequently encountered after abdominal or spinal surgeries. The condition leads to delayed gastrointestinal recovery, prolonged hospital stays, increased healthcare costs, and elevated morbidity. Therefore, robust preventive measures are essential to mitigate the onset and severity of this postoperative complication.
Risk Factors Necessitating Preventive Intervention
Successful prevention of paralytic ileus begins with identification of high-risk individuals. Factors include:
- Extensive intra-abdominal or pelvic surgeries
- Use of opioid analgesics
- Advanced age
- Electrolyte imbalances
- Systemic infection or sepsis
- Prolonged immobility
- Prior history of ileus
- Gastrointestinal inflammation (e.g., peritonitis, pancreatitis)
Core Prevention Strategies for Paralytic Ileus
Enhanced Recovery After Surgery (ERAS) Protocols
Implementation of ERAS protocols has demonstrated a substantial reduction in paralytic ileus incidence. Core components include:
- Minimally invasive surgery to reduce bowel manipulation
- Preoperative counseling and nutrition optimization
- Avoidance of routine nasogastric decompression
- Standardized fluid management to prevent bowel edema
- Multimodal analgesia to reduce reliance on opioids
- Early mobilization and feeding to stimulate gastrointestinal function
Minimizing Opioid Use with Multimodal Analgesia
Opioid analgesics are among the primary contributors to postoperative ileus due to their suppressive effect on gut motility. Multimodal pain management combines multiple non-opioid agents and techniques, including:
- Acetaminophen and NSAIDs
- Gabapentinoids
- Local anesthetic blocks (e.g., TAP block)
- Intravenous lidocaine or ketamine in selected cases
These alternatives reduce opioid requirement, preserving bowel function and enhancing recovery.
Alvimopan: Targeted Pharmacologic Prophylaxis
Alvimopan, a peripherally acting μ-opioid receptor antagonist, has proven efficacy in reducing postoperative ileus duration in patients undergoing bowel resection. It blocks opioid-induced gut motility suppression without affecting central analgesia.
- Indication: Short-term use in hospitalized patients
- Administration: Typically initiated preoperatively and continued postoperatively
- Benefit: Shortened time to first bowel movement and discharge
Correction of Electrolyte Imbalances
Intestinal motility is critically dependent on electrolyte balance. Prior to surgery and during recovery, the following must be monitored and corrected:
- Hypokalemia
- Hypomagnesemia
- Hyponatremia
- Hypercalcemia
Electrolyte optimization ensures smooth muscle excitability and neuromuscular coordination within the gastrointestinal tract.
Early Enteral Nutrition and Bowel Stimulation
Contrary to traditional practices of delayed feeding, early enteral nutrition encourages peristalsis and promotes mucosal integrity.
- Clear liquids may be initiated as early as 6 hours post-surgery
- Progression to solids is guided by patient tolerance
- Chewing gum has been shown to stimulate vagal activity, enhancing bowel motility through sham feeding
Early Ambulation: A Non-Pharmacologic Cornerstone
Prolonged bed rest contributes to delayed gastrointestinal recovery. Early postoperative mobilization accelerates return of bowel function and reduces complications.
- Begin ambulation within 24 hours post-surgery
- Encourage sitting upright and walking regularly
- Avoid prolonged recumbency
Mobilization also improves respiratory function and lowers thromboembolic risk, contributing to comprehensive recovery.
Role of Surgical Techniques in Preventing Ileus
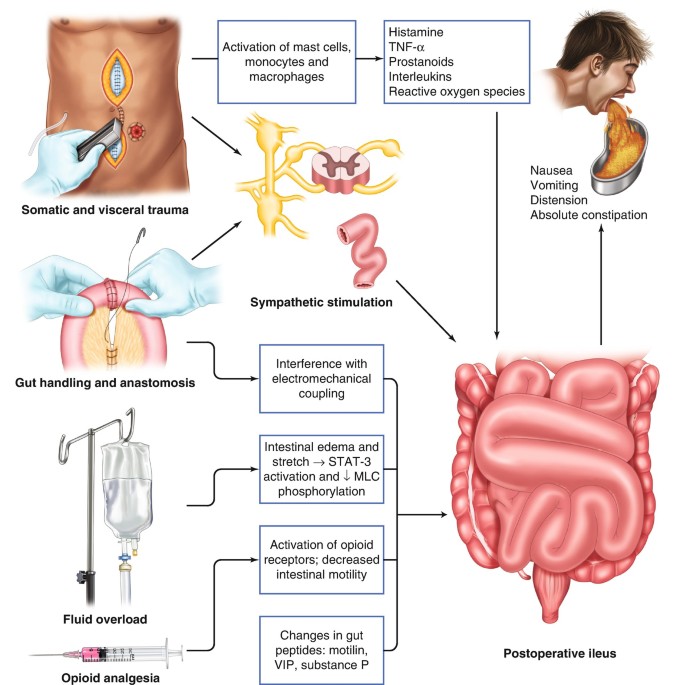
The degree of bowel manipulation, intraoperative trauma, and fluid shifts directly influence postoperative ileus.
Laparoscopic and Robotic-Assisted Surgery
- Minimizes tissue trauma and inflammation
- Reduces operative stress on the bowel
- Promotes faster return to normal GI function
Gentle Tissue Handling and Shorter Surgical Duration
- Decrease neuromuscular inhibition
- Lower activation of inhibitory reflex pathways
- Prevent excessive inflammatory cytokine release
Nursing Interventions to Support Prevention
Nursing teams play a critical role in monitoring and executing preventive measures:
- Regular abdominal assessments
- Bowel sound auscultation
- Monitoring stool and flatus passage
- Patient education on mobility and nutrition
- Pain control with minimal opioid use
Surveillance and Continuous Monitoring
Prevention of paralytic ileus is not static—it requires dynamic evaluation:
- Daily abdominal examinations
- Timely detection of ileus symptoms
- Immediate cessation of oral intake if ileus signs arise
- Prompt imaging to rule out mechanical obstruction
Continuous evaluation ensures that early interventions can be made before full ileus develops.
Frequently Asked Questions:
What is the most effective way to prevent paralytic ileus after surgery?
A combination of ERAS protocols, early mobilization, opioid-sparing analgesia, and electrolyte management offers the most effective prevention.
Can chewing gum help prevent ileus?
Yes, chewing gum acts as a form of sham feeding, stimulating the gastrointestinal tract via the vagus nerve and reducing the duration of ileus.
When should Alvimopan be used?
Alvimopan is indicated for high-risk patients undergoing bowel resection. It should be started before surgery and continued postoperatively under supervision.
How soon should patients eat after abdominal surgery?
In the absence of contraindications, clear liquids can be initiated within 6–12 hours postoperatively, progressing as tolerated.
Why is electrolyte correction important in ileus prevention?
Electrolytes like potassium and magnesium are essential for muscle contractions in the bowel. Imbalances may delay peristalsis.
Preventing paralytic ileus requires an integrative, multidisciplinary approach that begins before the first incision and extends through the postoperative period. By implementing evidence-based strategies—ranging from surgical technique refinement to enhanced recovery protocols—we significantly reduce the incidence and burden of this condition. Through early intervention, optimal pain control, and vigilant monitoring, patients can experience faster gastrointestinal recovery, fewer complications, and shorter hospital stays.