Paragangliomas are rare, typically benign neuroendocrine tumors arising from the paraganglia—a collection of chromaffin cells located outside the adrenal glands. These tumors are closely related to pheochromocytomas, which occur within the adrenal medulla. While many paragangliomas are nonfunctional, some produce catecholamines, leading to significant clinical manifestations.
Paragangliomas are classified based on their location:
- Sympathetic paragangliomas (often functional): Thoracic, abdominal, and pelvic
- Parasympathetic paragangliomas (usually nonfunctional): Head and neck regions
Etiology and Genetic Predisposition
Approximately 30–40% of paragangliomas are associated with hereditary syndromes. Key genetic mutations involved include:
- SDHx gene mutations (SDHB, SDHD, SDHC, SDHA, SDHAF2)
- VHL (Von Hippel–Lindau)
- RET proto-oncogene (Multiple Endocrine Neoplasia type 2)
- NF1 gene (Neurofibromatosis type 1)
Inheritance Patterns
Most inherited mutations follow an autosomal dominant pattern. Mutations in SDHB are associated with higher metastatic potential and poorer prognosis.
Pathophysiology and Tumor Biology
Paragangliomas originate from neuroectodermal chromaffin cells that are part of the autonomic nervous system. Sympathetic tumors often secrete excessive norepinephrine and epinephrine, while parasympathetic tumors rarely produce hormones.
Clinical Presentation and Symptoms
Functional Paragangliomas
These tumors secrete catecholamines and manifest as:
- Hypertension (sustained or paroxysmal)
- Palpitations
- Diaphoresis
- Headaches
- Anxiety or panic attacks
- Pallor
- Orthostatic hypotension
Nonfunctional Paragangliomas
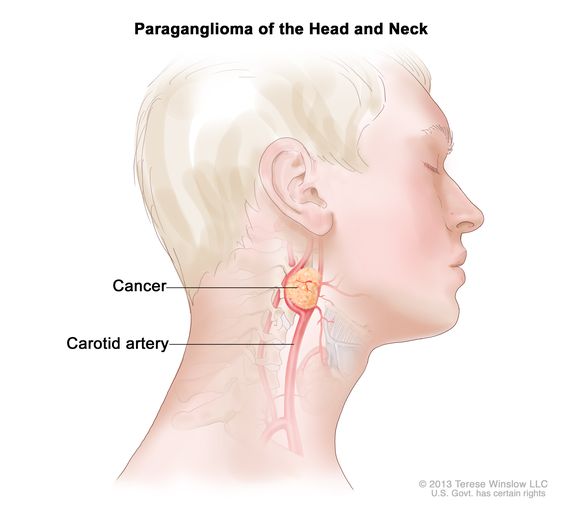
Most often located in the head and neck, including:
- Carotid body tumor
- Jugulotympanic paraganglioma
- Vagal paraganglioma
Symptoms depend on tumor size and location:
- Neck mass
- Dysphagia
- Hoarseness
- Pulsatile tinnitus
- Cranial nerve deficits (IX–XII)
Diagnostic Evaluation
Biochemical Testing
- Plasma free metanephrines
- 24-hour urinary fractionated metanephrines and catecholamines
Elevated levels confirm catecholamine-secreting tumors.
Imaging Studies
- MRI or CT scan: Identify tumor location and size
- 123I-MIBG scintigraphy: Useful for functional imaging
- PET scan with 68Ga-DOTATATE or FDG: For metastatic disease and SDHB-related tumors
Genetic Testing
Recommended for all patients due to high heritability. Early identification helps in surveillance of family members.
Histopathology and Classification
Paragangliomas exhibit a characteristic zellballen (nest-like) pattern on microscopy, with sustentacular cells stained by S-100.
| Histological Feature | Description |
|---|---|
| Zellballen pattern | Nests of chief cells surrounded by stroma |
| Sustentacular cells | S-100 positive, supportive cell layer |
| Chromogranin and Synaptophysin | Positive in chief cells |
Staging and Malignancy
Paragangliomas are considered malignant only when metastases are present, as no histological marker can predict malignancy. Metastatic sites include:
- Lymph nodes
- Bone
- Liver
- Lungs
Treatment and Management Strategies
Surgical Resection
Primary treatment for localized paraganglioma. Preoperative management includes:
- Alpha-adrenergic blockade (e.g., phenoxybenzamine)
- Beta-blockade (only after adequate alpha-blockade)
- High-sodium diet and fluid replacement
Radiation Therapy
Used for:
- Inoperable tumors
- Residual or recurrent head and neck paragangliomas
- Palliative treatment of metastases
Medical Therapy
- MIBG therapy for MIBG-avid tumors
- Somatostatin analogs for tumors expressing somatostatin receptors
- Chemotherapy: Cyclophosphamide, vincristine, and dacarbazine (CVD regimen) for progressive metastatic disease
Follow-up and Prognosis
Lifelong follow-up is essential due to risk of recurrence and metastasis. Recommended surveillance includes:
- Annual plasma metanephrine testing
- Periodic imaging (MRI/CT)
- Genetic counseling for patients and families
Prognosis
- Benign tumors: Excellent prognosis with complete resection
- SDHB mutation-related tumors: Higher risk of malignancy and poorer outcomes
- Metastatic disease: Managed as a chronic condition, variable survival depending on response to treatment
Complications
- Crisis during surgery due to catecholamine surge
- Cranial nerve injury in head and neck tumors
- Hypertensive emergencies in functional tumors
- Tumor recurrence or metastasis
Prevention and Genetic Counseling
Due to the strong genetic component, early identification of mutation carriers is critical. Genetic counseling should include:
- Discussion of testing implications
- Family screening
- Prenatal options in familial syndromes
Frequently Asked Questions
Is paraganglioma cancerous?
Paragangliomas are generally benign. However, they are labeled malignant only if metastases are present.
How is paraganglioma different from pheochromocytoma?
Both are chromaffin-cell tumors. Pheochromocytomas occur in the adrenal medulla, while paragangliomas are extra-adrenal.
Can paragangliomas recur?
Yes. Recurrence may occur even after complete surgical excision, particularly in hereditary cases.
What is the survival rate for malignant paraganglioma?
Long-term survival varies based on metastatic burden and response to therapy. Some patients live for years with managed disease.
Are paragangliomas inherited?
Yes. Up to 40% are hereditary, especially those associated with SDHx mutations and other syndromic conditions.