Pancreatic neuroendocrine tumors (pNETs) are a rare subset of pancreatic neoplasms that originate from the hormone-producing islet cells of the pancreas. Unlike the more common pancreatic adenocarcinoma, pNETs tend to have a slower progression but can still be malignant and potentially life-threatening. These tumors can be either functioning, secreting hormones that cause clinical syndromes, or non-functioning, which typically present later due to mass effect.
Classification of pNETs by Functionality and Grade
Functioning vs. Non-functioning pNETs
- Functioning Tumors: These secrete active hormones such as insulin, gastrin, glucagon, vasoactive intestinal peptide (VIP), or somatostatin.
- Non-functioning Tumors: These do not secrete biologically active hormones and are often diagnosed incidentally or through symptoms related to mass effect.
Grading by Tumor Proliferation
The World Health Organization (WHO) classifies pNETs based on mitotic count and Ki-67 proliferation index:
| Grade | Mitotic Count (per 10 HPF) | Ki-67 Index | Description |
|---|---|---|---|
| G1 | <2 | ≤2% | Well-differentiated, slow-growing |
| G2 | 2–20 | 3–20% | Intermediate grade |
| G3 | >20 | >20% | High grade, aggressive |
Pathophysiology and Molecular Basis of pNET
pNETs arise from the diffuse neuroendocrine system within the pancreas. Genetic mutations commonly associated with pNETs include:
- MEN1 gene mutation – seen in Multiple Endocrine Neoplasia type 1
- DAXX and ATRX mutations – associated with chromatin remodeling
- mTOR pathway mutations – impacting cell growth and metabolism
Clinical Presentation of Pancreatic Neuroendocrine Tumors
Functioning pNETs and Their Syndromes
- Insulinoma: Hypoglycemia, confusion, sweating
- Gastrinoma (Zollinger-Ellison Syndrome): Peptic ulcers, diarrhea
- Glucagonoma: Diabetes, necrolytic migratory erythema
- VIPoma: Profuse watery diarrhea, hypokalemia
- Somatostatinoma: Diabetes, gallstones, steatorrhea
Non-functioning pNETs
Non-functioning tumors are often discovered incidentally or present late with:
- Abdominal pain
- Jaundice
- Weight loss
- Obstruction of bile or pancreatic ducts
Diagnostic Strategies for pNET
Biochemical Testing
- Hormonal assays (insulin, gastrin, VIP, glucagon, chromogranin A)
- Fasting glucose and C-peptide (for insulinomas)
- 24-hour urinary 5-HIAA (to rule out carcinoid syndrome)
Imaging Modalities
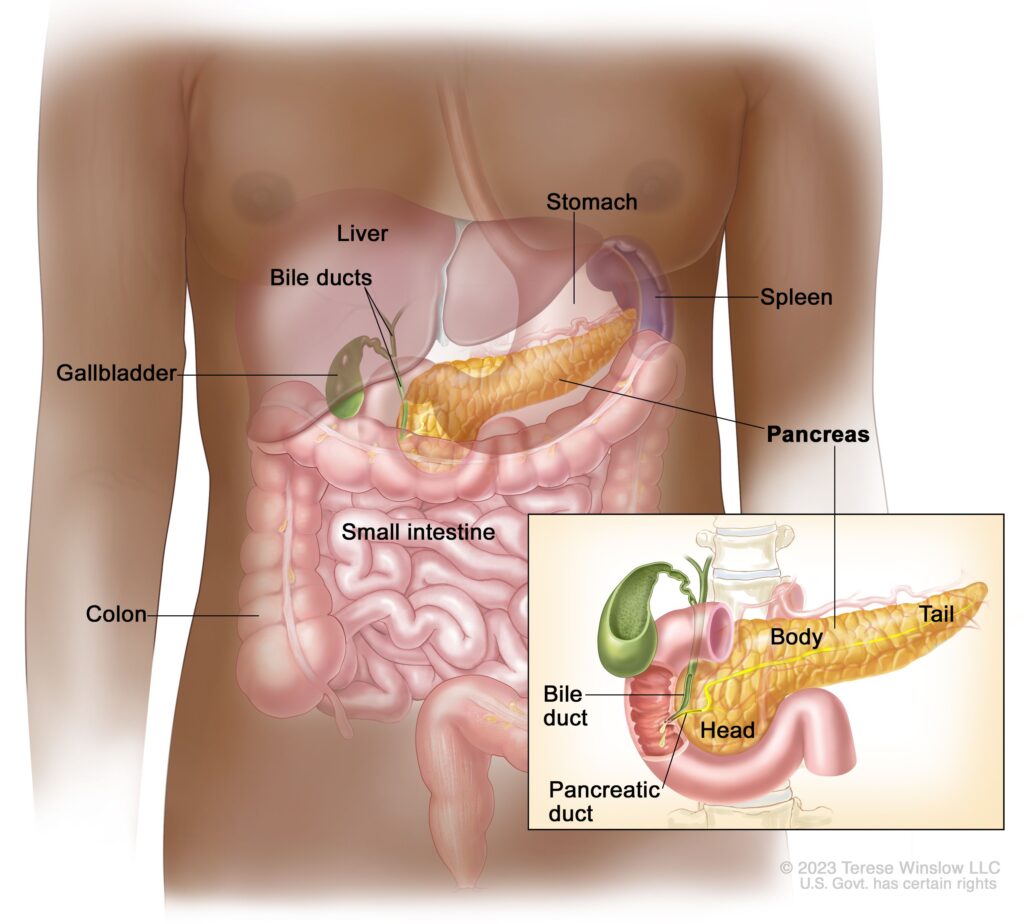
- CT and MRI scans: For anatomical localization and staging
- Somatostatin receptor scintigraphy (Octreoscan)
- Gallium-68 DOTATATE PET/CT: Superior for detecting somatostatin receptor-positive tumors
- Endoscopic ultrasound (EUS): Ideal for small lesions and biopsy acquisition
Histopathology
- Fine needle aspiration (FNA) or core biopsy
- Immunohistochemical staining: Chromogranin A, synaptophysin, Ki-67
Therapeutic Approaches for pNET
Surgical Management
Surgery remains the only curative option for localized pNETs:
- Enucleation: For small, benign lesions
- Pancreaticoduodenectomy (Whipple procedure): For tumors in the head of the pancreas
- Distal pancreatectomy: For tumors in the body or tail
Medical Therapies
- Somatostatin analogs (Octreotide, Lanreotide): Control symptoms and slow tumor progression
- Targeted therapies:
- Everolimus: mTOR inhibitor
- Sunitinib: Tyrosine kinase inhibitor
- Chemotherapy: Streptozocin, doxorubicin, temozolomide used for high-grade or metastatic cases
Peptide Receptor Radionuclide Therapy (PRRT)
- Utilizes radiolabeled somatostatin analogs (e.g., Lutetium-177 DOTATATE)
- Effective for advanced, inoperable, or metastatic pNETs with somatostatin receptor expression
Prognosis and Survival Outcomes
Prognosis varies based on tumor grade, functionality, and metastatic spread:
| Factor | Prognosis |
|---|---|
| Localized, low-grade | >80% 5-year survival |
| Regional metastasis | ~60% 5-year survival |
| Distant metastasis | ~30% 5-year survival |
| Functioning tumors | Often detected earlier, better prognosis |
| High Ki-67 index | Associated with aggressive behavior |
Regular surveillance and follow-up imaging are essential due to the risk of recurrence and progression.
Emerging Research and Future Directions
- Immunotherapy is under evaluation, though efficacy remains limited for most pNETs.
- Liquid biopsies for circulating tumor DNA (ctDNA) and cell-free RNA offer promise for early detection and treatment monitoring.
- Artificial intelligence and radiomics may enhance diagnostic precision in imaging.
- Next-generation sequencing (NGS) enables personalized therapy by identifying actionable mutations.
Frequently Asked Questions
What is the difference between pancreatic neuroendocrine tumors and pancreatic adenocarcinoma?
pNETs arise from endocrine cells and often grow more slowly, whereas adenocarcinomas arise from ductal cells and are more aggressive.
Are all pancreatic neuroendocrine tumors cancerous?
Not all are malignant. Many are benign or low-grade, but some may be locally invasive or metastatic.
How common is pNET?
They account for less than 5% of all pancreatic tumors, making them relatively rare.
Can pNET be cured?
Surgical resection can be curative if detected early. For advanced disease, therapies aim to control symptoms and progression.
Is genetic testing recommended?
Yes, especially if associated with hereditary syndromes such as MEN1 or in younger patients.