Ovulation stimulation is a pivotal component in fertility treatment protocols aimed at enhancing a woman’s chances of conceiving. By pharmacologically inducing or regulating ovulation, we can increase the number of mature oocytes available for fertilization during timed intercourse, intrauterine insemination (IUI), or in vitro fertilization (IVF). Understanding the types, medications, monitoring strategies, and potential outcomes of ovulation stimulation is essential for optimizing reproductive success.
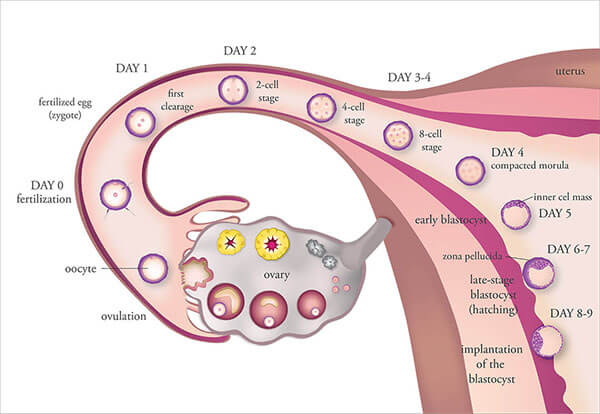
Understanding the Physiology of Ovulation
Ovulation is the culmination of a finely regulated hormonal cycle, primarily governed by:
- Follicle-Stimulating Hormone (FSH) – Stimulates growth of ovarian follicles.
- Luteinizing Hormone (LH) – Triggers ovulation and corpus luteum formation.
- Estrogen and Progesterone – Regulate endometrial preparation and cycle feedback.
In women with ovulatory dysfunction, this endocrine balance is disrupted, necessitating medical intervention to restore or enhance ovulatory function.
Indications for Ovulation Stimulation
We recommend ovulation stimulation in the following clinical scenarios:
- Anovulation or Oligo-ovulation: Common in conditions such as polycystic ovary syndrome (PCOS).
- Unexplained infertility: To enhance the probability of oocyte release.
- Assisted reproductive technologies (ART): Including IVF and IUI.
- Diminished ovarian reserve: To retrieve multiple oocytes for fertilization.
- Endocrine disorders: Such as hypothalamic amenorrhea or luteal phase defects.
Pharmacologic Agents Used in Ovulation Stimulation
Clomiphene Citrate (CC)
- Mechanism: Selective estrogen receptor modulator (SERM) that induces FSH and LH surge via hypothalamic stimulation.
- Protocol: 50–150 mg/day for 5 days starting on day 2–5 of the menstrual cycle.
- Indications: First-line treatment in women with PCOS or unexplained infertility.
- Success Rate: Ovulation in ~80%, pregnancy in ~40% over 6 cycles.
Letrozole
- Mechanism: Aromatase inhibitor that reduces estrogen synthesis, enhancing FSH production.
- Advantages: Better endometrial receptivity and mono-follicular response compared to clomiphene.
- Use: Increasingly preferred in PCOS-related ovulatory dysfunction.
Gonadotropins (FSH, hMG)
- Mechanism: Direct ovarian stimulation via exogenous FSH/LH.
- Protocols: Step-up, step-down, or low-dose regimens.
- Risks: Higher incidence of multiple pregnancies and ovarian hyperstimulation syndrome (OHSS).
Human Chorionic Gonadotropin (hCG)
- Function: Mimics the natural LH surge to induce final follicular maturation and ovulation.
- Timing: Administered when lead follicle reaches 18–20 mm diameter.
Monitoring of Ovulation Stimulation
Monitoring is critical to assess response and minimize risks. Common modalities include:
- Transvaginal Ultrasonography: To measure follicular development and endometrial thickness.
- Serum Estradiol (E2): Reflects follicular activity; used in gonadotropin cycles.
- LH and Progesterone Levels: To confirm ovulation and luteal adequacy.
Ovulation Stimulation Protocols in IVF
Controlled Ovarian Hyperstimulation (COH)
Used to maximize oocyte yield in IVF, COH involves:
- GnRH Agonist or Antagonist Protocols: Prevent premature LH surge.
- Recombinant FSH or hMG: Administered daily.
- hCG or GnRH agonist trigger: Given once follicles are mature.
Oocyte Retrieval
Typically performed 34–36 hours post-hCG injection via ultrasound-guided transvaginal aspiration.
Risks and Complications of Ovulation Stimulation
While effective, ovulation stimulation carries certain risks:
- Ovarian Hyperstimulation Syndrome (OHSS): Characterized by enlarged ovaries, ascites, and fluid imbalance.
- Multiple Gestations: Especially with gonadotropins; associated with preterm labor and maternal complications.
- Cyst Formation or Ovarian Torsion
- Psychological Stress and Cost Burden
Strategies to Minimize Risks
- Individualized Protocols: Adjusting doses based on age, BMI, and ovarian reserve.
- Low-Dose Step-Up Regimens: Especially in PCOS patients.
- Cycle Cancellation: If excessive follicles develop or OHSS risk is high.
- Single Embryo Transfer (SET): To reduce multiple gestation risks in IVF.
Success Rates and Prognostic Factors
Influencing Factors
- Age of the patient
- Cause of infertility
- Duration of infertility
- Ovarian reserve (AMH, AFC)
- BMI and metabolic status
Expected Outcomes
- Ovulation Rate: >70% with most agents.
- Pregnancy Rate per Cycle: 15–25% with oral agents; up to 40% with IVF.
- Live Birth Rate: Cumulative success increases over multiple cycles.
Lifestyle and Complementary Approaches
- Weight Management: Crucial in PCOS; even 5–10% weight loss improves ovulatory response.
- Nutritional Optimization: Antioxidant-rich diet supports oocyte health.
- Stress Reduction: Mind-body programs, yoga, and counseling may improve hormonal balance.
- Supplements: Myo-inositol, folic acid, and CoQ10 are commonly advised.
Frequently Asked Questions:
What is ovulation stimulation?
A medical process that uses medications to induce or regulate ovulation, especially in women with infertility.
Is ovulation stimulation the same as IVF?
No. Ovulation stimulation may be part of IVF, but it can also be used for simpler methods like timed intercourse or IUI.
Can ovulation stimulation cause twins?
Yes, particularly with gonadotropin therapy. Letrozole and clomiphene have lower, but still elevated, multiple pregnancy rates.
How is ovulation monitored during stimulation?
Through serial ultrasound scans and hormone blood tests (E2, LH, progesterone).
How many cycles can I undergo?
Up to 6 cycles with oral agents like clomiphene is typical. For gonadotropins or IVF, the number depends on response and medical advice.
Ovulation stimulation is a cornerstone in the management of infertility, offering hope to millions of women with ovulatory disorders or unexplained infertility. Through appropriate selection of pharmacologic agents, individualized dosing, and vigilant monitoring, we can enhance ovulatory outcomes, improve pregnancy rates, and ensure safety throughout the treatment process. By combining clinical expertise with patient-centered care, ovulation stimulation remains an effective and evolving strategy in the journey toward parenthood.