Ovarian germ cell tumor carcinoma encompasses a rare but aggressive category of ovarian malignancies originating from primordial germ cells. These tumors primarily affect adolescents and young women under the age of 30, making early detection and tailored treatment essential for survival and fertility preservation. Although accounting for less than 5% of all ovarian cancers, malignant ovarian germ cell tumors (MOGCTs) require specialized diagnostic and therapeutic strategies.
Classification of Malignant Ovarian Germ Cell Tumors
Major Histological Subtypes
Ovarian germ cell carcinomas can be divided into distinct malignant variants:
- Dysgerminoma: Most common and least aggressive, accounting for ~30–40% of MOGCTs.
- Endodermal Sinus Tumor (Yolk Sac Tumor): Rapidly growing and highly malignant.
- Immature Teratoma: Contains immature embryonic tissue, often neuroectodermal.
- Choriocarcinoma (Non-gestational): Rare and aggressive, produces high hCG.
- Mixed Germ Cell Tumors: Contain more than one histological component.
Risk Factors and Etiology
While most cases are sporadic, certain factors may increase susceptibility:
- Age under 30 years
- Genetic syndromes such as Swyer syndrome or gonadal dysgenesis
- Family history of germ cell tumors
- Presence of gonadal dysgenesis or abnormal karyotypes (e.g., 46,XY)
Clinical Presentation: Recognizing the Symptoms
Due to their rapid growth, ovarian germ cell carcinomas often present acutely:
- Pelvic or abdominal pain
- Palpable abdominal mass
- Abdominal distension or bloating
- Abnormal uterine bleeding
- Symptoms of hormone secretion, such as precocious puberty or virilization
Advanced tumors may present with ascites or metastatic symptoms if not detected early.
Diagnostic Workup of Ovarian Germ Cell Tumors
Serum Tumor Markers
Tumor markers play a vital role in both diagnosis and monitoring:
- Alpha-fetoprotein (AFP): Elevated in yolk sac tumors.
- Beta-human chorionic gonadotropin (β-hCG): High in choriocarcinoma and some mixed tumors.
- Lactate dehydrogenase (LDH): Marker for dysgerminoma.
- CA-125: May be raised nonspecifically.
Imaging Studies
- Ultrasound (TVS/Abdominal): First-line for pelvic mass identification.
- MRI/CT scan: Used to evaluate tumor extent and staging.
- PET-CT: Occasionally employed in staging or recurrence evaluation.
Histopathological Examination and Staging
Surgical Biopsy and Histology
Definitive diagnosis is established via histological analysis post-surgical biopsy or tumor excision. Common features include:
- Dysgerminoma: Sheets of uniform cells with clear cytoplasm and lymphocytic infiltration.
- Yolk Sac Tumor: Schiller-Duval bodies are pathognomonic.
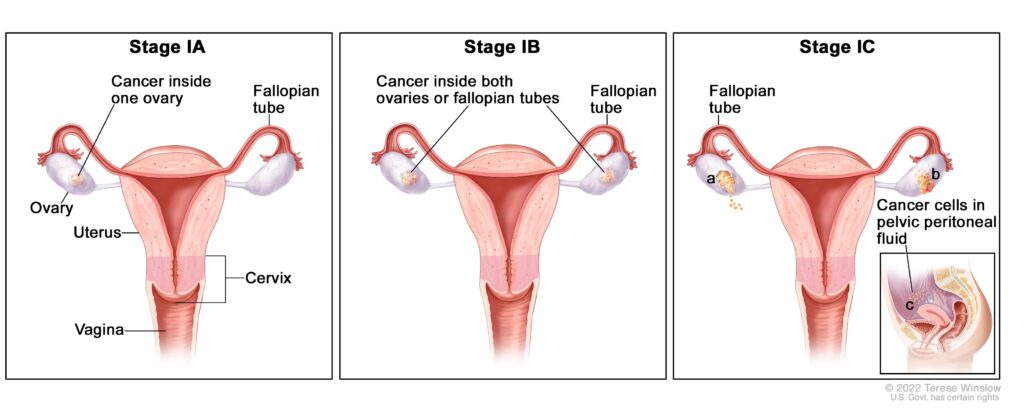
FIGO Staging for Ovarian Germ Cell Carcinomas
- Stage I: Confined to the ovaries.
- Stage II: Spread to pelvic structures.
- Stage III: Involvement of peritoneum or lymph nodes.
- Stage IV: Distant metastases (e.g., lung, liver).
Treatment of Ovarian Germ Cell Tumor Carcinoma
Surgical Management
- Fertility-Sparing Surgery: Unilateral salpingo-oophorectomy for early-stage, preserving uterus and contralateral ovary.
- Comprehensive Surgical Staging: Includes lymph node sampling, omentectomy, and peritoneal biopsies.
- Debulking Surgery: For advanced disease, aiming for no residual tumor.
Chemotherapy
BEP Regimen (Bleomycin, Etoposide, Cisplatin): Standard first-line treatment.
- Cycles: Typically 3–4 cycles for Stage I high-risk or advanced tumors.
- Response Rate: >90% complete remission in early-stage disease.
- Toxicities: Pulmonary fibrosis (Bleomycin), nephrotoxicity, and myelosuppression.
Radiotherapy
Rarely used, as germ cell tumors are generally chemosensitive. May be considered in dysgerminomas unresponsive to chemotherapy.
Prognosis and Long-Term Outcomes
Survival Rates
- Stage I dysgerminoma: >95% 5-year survival
- Stage III/IV mixed tumors: 70–80% with chemotherapy
Recurrence
Most relapses occur within 2 years; hence close surveillance with tumor markers and imaging is crucial.
Fertility Preservation and Reproductive Outcomes
- Fertility-sparing approaches are feasible and safe in the majority of cases.
- Menstrual cycles resume post-chemotherapy in ~85% of cases.
- Pregnancy outcomes are generally favorable post-treatment, even in patients who received BEP chemotherapy.
Surveillance After Treatment
Regular follow-up is necessary due to recurrence risk:
- Physical exams: Every 3 months for 2 years, then every 6–12 months.
- Tumor markers: AFP, β-hCG, LDH levels monitored routinely.
- Imaging: Annual or symptom-directed.
Emerging Therapies and Research Directions
- Targeted therapies: Trials exploring anti-angiogenic agents, mTOR inhibitors.
- Genetic profiling: Identification of biomarkers for tailored treatment.
- Minimally invasive surgery: Gaining favor for staging in early-stage disease.
Frequently Asked Questions:
What age group is most affected by ovarian germ cell tumor carcinoma?
Typically affects adolescents and young women under 30 years of age.
Can these tumors be cured?
Yes, with appropriate surgery and chemotherapy, most cases are curable, even in advanced stages.
Is fertility preserved after treatment?
In most patients, especially with fertility-sparing surgery and limited chemotherapy exposure, fertility can be maintained.
How fast do these tumors grow?
They are generally fast-growing, which is why early detection is critical.
Are germ cell tumors hereditary?
Most are sporadic; however, rare associations with genetic syndromes exist.
Ovarian germ cell tumor carcinoma, though rare, constitutes a critical entity in gynecologic oncology due to its aggressive nature and impact on young women. With advancements in surgical techniques, chemotherapeutic regimens, and fertility preservation, long-term survival with optimal quality of life is increasingly achievable. Early diagnosis through symptom recognition and tumor marker analysis, coupled with multidisciplinary management, remains the cornerstone of success in treating these malignancies.