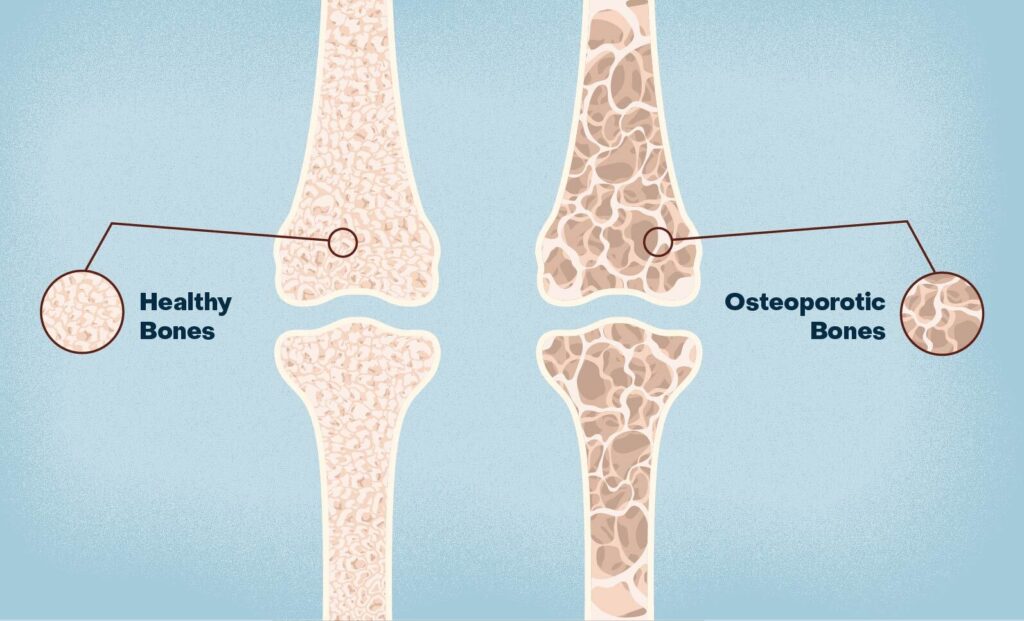
Osteoporosis is a progressive skeletal disorder characterized by decreased bone mass and deterioration of bone tissue, leading to enhanced bone fragility and an increased risk of fractures. This condition affects millions worldwide, particularly postmenopausal women and the elderly, contributing significantly to morbidity, mortality, and healthcare costs.
The Science of Bone Remodeling and Osteoporosis
Bone tissue undergoes continuous remodeling, involving the balanced processes of bone resorption by osteoclasts and bone formation by osteoblasts. In osteoporosis, this balance is disrupted, favoring resorption, which weakens the bone structure.
Key Causes and Risk Factors of Osteoporosis
1. Hormonal Changes
- Estrogen deficiency in postmenopausal women accelerates bone loss.
- Androgen deficiency in men also contributes, though less commonly.
2. Nutritional Deficiencies
- Inadequate calcium and vitamin D intake impairs bone mineralization.
- Excessive alcohol and caffeine reduce calcium absorption.
3. Sedentary Lifestyle
- Lack of weight-bearing exercise weakens bones and muscles.
4. Medical Conditions and Medications
- Hyperthyroidism, chronic kidney disease, and malabsorption syndromes.
- Long-term use of corticosteroids, anticonvulsants, and heparin.
5. Genetic and Demographic Factors
- Family history, female gender, advanced age, and Caucasian or Asian ethnicity elevate risk.
Recognizing Symptoms and Complications
Osteoporosis is often asymptomatic until a fracture occurs. Common clinical manifestations include:
- Fractures: Especially in the spine, hip, and wrist.
- Loss of Height: Caused by vertebral compression fractures.
- Back Pain: Often due to collapsed or fractured vertebrae.
- Stooped Posture: Resulting from vertebral deformities.
Diagnostic Tools for Osteoporosis Detection
Bone Mineral Density (BMD) Testing
The Dual-Energy X-ray Absorptiometry (DEXA) scan is the gold standard for diagnosing osteoporosis. It measures BMD at the hip and spine and provides a T-score:
- Normal: T-score ≥ -1.0
- Osteopenia: T-score between -1.0 and -2.5
- Osteoporosis: T-score ≤ -2.5
Additional Tests
- FRAX Score: Calculates 10-year fracture risk using clinical factors.
- X-rays: Reveal existing fractures.
- Blood Tests: Assess calcium, vitamin D, thyroid, and renal function.
Effective Prevention Strategies for Osteoporosis
Nutritional Interventions
- Calcium: Adults aged 50+ require 1000–1200 mg/day.
- Vitamin D: 800–1000 IU/day enhances calcium absorption.
- Include dairy products, leafy greens, fortified foods, and supplements if needed.
Physical Activity
- Weight-bearing Exercises: Walking, jogging, dancing, and stair climbing.
- Resistance Training: Builds bone and muscle strength.
- Balance and Flexibility Training: Prevents falls.
Lifestyle Modifications
- Quit smoking and reduce alcohol consumption.
- Maintain a healthy weight.
- Regular fall-risk assessments for the elderly.
Medical Treatment Options for Osteoporosis
1. Bisphosphonates
Suppress bone resorption by inhibiting osteoclasts. Common agents include:
- Alendronate
- Risedronate
- Zoledronic acid
2. Selective Estrogen Receptor Modulators (SERMs)
- Raloxifene mimics estrogen’s protective effects on bone.
3. Hormone Replacement Therapy (HRT)
Effective in early postmenopausal women but used cautiously due to cardiovascular risks.
4. Parathyroid Hormone Analogs
- Teriparatide stimulates bone formation.
5. Monoclonal Antibodies
- Denosumab inhibits RANKL, a key factor in osteoclast development.
6. Calcium and Vitamin D Supplements
Essential as adjunct therapy to all pharmacological regimens.
Osteoporosis in Special Populations
Postmenopausal Women
- Most affected group due to estrogen deficiency.
- Screening recommended for all women aged 65+ or younger with risk factors.
Men
- Often underdiagnosed. Consider screening men over 70 or younger with risks.
Patients on Long-Term Steroids
- Require baseline and follow-up DEXA scans and prophylactic treatment.
Individuals with Secondary Causes
- Treat underlying disorders (e.g., celiac disease, hyperparathyroidism).
Complications and Fracture Management
Hip Fractures
- Associated with significant disability and mortality.
- Often require surgical repair and prolonged rehabilitation.
Vertebral Fractures
- May cause chronic pain, deformity, and reduced lung function.
- Vertebroplasty or kyphoplasty may be considered in selected cases.
Fall Prevention
- Home safety modifications, use of assistive devices, and vision correction reduce risk.
Prognosis and Quality of Life Considerations
Timely diagnosis and comprehensive management significantly reduce fracture risk and improve outcomes. A multidisciplinary approach involving physicians, dietitians, physiotherapists, and caregivers is crucial in maintaining bone health and enhancing quality of life.
Frequently Asked Questions:
What is the difference between osteopenia and osteoporosis?
Osteopenia is a precursor to osteoporosis with lower-than-normal bone density, but not low enough to meet osteoporosis criteria.
Can osteoporosis be reversed?
While not fully reversible, bone loss can be slowed or halted with proper treatment, and fracture risk can be significantly reduced.
Who should get a DEXA scan?
Women aged 65+, men aged 70+, and anyone with risk factors such as fractures or long-term steroid use.
What foods are best for osteoporosis?
Dairy, leafy greens, fortified cereals, fish with bones (like sardines), and eggs support bone health.
Is exercise safe for people with osteoporosis?
Yes, low-impact weight-bearing and strength-training exercises are recommended to maintain bone strength and balance.
Osteoporosis is a major public health concern with profound implications for aging populations. With appropriate prevention, early diagnosis, and targeted treatment, individuals can preserve bone density, minimize fracture risk, and lead active, healthy lives. Implementing a proactive, evidence-based approach is essential for long-term skeletal health and overall well-being.