Osteoarthritis (OA) of the knee is a degenerative joint disease characterized by the progressive breakdown of articular cartilage, subchondral bone remodeling, and inflammation of the synovium. As the most common form of arthritis affecting the knee joint, OA leads to pain, stiffness, swelling, and functional limitations, especially in older adults. The condition often worsens over time, significantly impacting quality of life and mobility.
Causes and Risk Factors for Knee Osteoarthritis
Primary vs Secondary Osteoarthritis
- Primary OA occurs due to age-related wear and tear with no identifiable cause.
- Secondary OA results from factors such as trauma, joint instability, metabolic diseases, or congenital abnormalities.
Common Risk Factors
- Age: Prevalence increases with age due to cumulative cartilage wear.
- Obesity: Excess body weight increases mechanical stress on the knee joint.
- Genetics: Family history can predispose individuals to OA.
- Injury History: Previous ligament or meniscal injuries elevate risk.
- Occupational/Repetitive Stress: Jobs involving kneeling, squatting, or heavy lifting.
- Joint Malalignment: Abnormal biomechanics due to varus or valgus deformities.
Anatomy of the Knee and Pathophysiology of OA
The knee comprises three compartments: medial, lateral, and patellofemoral. OA may affect one or more of these compartments, leading to unicompartmental or tricompartmental OA.
Key Pathological Changes
- Cartilage degradation
- Subchondral bone sclerosis
- Osteophyte (bone spur) formation
- Joint space narrowing
Clinical Symptoms of Knee Osteoarthritis
Symptoms typically develop gradually and worsen over time.
- Pain: Often worsens with activity and improves with rest.
- Stiffness: Especially after prolonged inactivity (morning stiffness <30 minutes).
- Swelling: Due to synovial inflammation or joint effusion.
- Crepitus: A grating sensation during joint movement.
- Limited Range of Motion
- Deformity: Advanced OA may cause bowing (varus) or knock-knees (valgus).
Diagnostic Evaluation of Knee OA
Clinical Assessment
A thorough history and physical examination are the initial steps. Key findings include tenderness, crepitus, joint line pain, and reduced motion.
Imaging Techniques
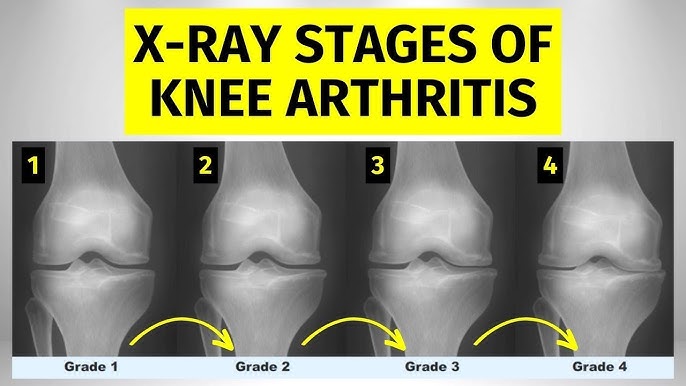
- X-ray: Most common tool. Reveals joint space narrowing, osteophytes, and subchondral sclerosis.
- MRI: Useful in early disease to detect cartilage loss, bone marrow lesions, or meniscal damage.
- Ultrasound: Assists in detecting effusion and guiding injections.
Diagnostic Criteria
According to the American College of Rheumatology (ACR):
- Age ≥50 years
- Crepitus on active motion
- Morning stiffness <30 minutes
- Bony tenderness or enlargement
- No palpable warmth over the joint
Non-Surgical Treatment Options for Knee OA
Lifestyle Modifications
- Weight Management: Reduces joint load and progression of OA.
- Exercise: Strengthening quadriceps and improving flexibility reduces pain and improves function.
Physical Therapy
Tailored programs focusing on balance, proprioception, and gait correction enhance joint stability.
Assistive Devices
- Canes or walkers: Reduce joint load.
- Bracing: Offloads the affected compartment in unicompartmental OA.
Pharmacologic Therapy
- Acetaminophen: First-line for mild pain.
- NSAIDs: More effective for inflammation and moderate pain; use with caution due to GI and cardiovascular risks.
- Topical NSAIDs: Safer alternative for localized symptoms.
- Intra-articular Injections:
- Corticosteroids: Provide short-term relief of inflammation.
- Hyaluronic Acid: Viscosupplementation for lubrication and cushioning.
Emerging Therapies
- Platelet-Rich Plasma (PRP): Regenerative potential in early OA.
- Stem Cell Therapy: Still under investigation but offers promise.
Surgical Treatment for Advanced Knee OA
Indications for Surgery
Persistent pain, deformity, or functional decline unresponsive to conservative measures.
Surgical Options
- Arthroscopy: Limited role; may be used for meniscal repair or debridement in select cases.
- Osteotomy: Realignment surgery for younger patients with unicompartmental OA.
- Unicompartmental Knee Replacement: Replaces only the damaged compartment, preserving bone and ligaments.
- Total Knee Arthroplasty (TKA): Gold standard for severe, tricompartmental OA.
Post-Surgical Rehabilitation
- Early mobilization
- Physical therapy for range of motion and strength
- Long-term functional training
Prognosis and Long-Term Outlook
Knee osteoarthritis is a chronic condition with a variable course. While it cannot be reversed, early diagnosis and comprehensive management can slow progression, reduce pain, and maintain quality of life. Surgical options provide definitive relief in end-stage disease.
Prevention Strategies for Knee Osteoarthritis
- Maintain healthy body weight
- Avoid repetitive knee strain
- Engage in regular low-impact exercise (e.g., swimming, cycling)
- Protect knees from injury through proper techniques during sports
- Address joint malalignment early
Frequently Asked Questions:
Is knee osteoarthritis curable?
Knee OA is not curable, but symptoms can be managed effectively through a combination of therapies.
What is the best treatment for knee osteoarthritis?
There is no one-size-fits-all treatment. A combination of lifestyle changes, medications, physical therapy, and sometimes surgery offers the best results.
How do I know if my knee pain is from osteoarthritis?
If your knee pain worsens with activity, improves with rest, and is associated with stiffness and swelling, OA may be the cause. Imaging can confirm the diagnosis.
Can walking worsen knee OA?
Walking improves joint function and should be encouraged unless it causes significant pain. Proper footwear and terrain matter.
What exercises are best for knee OA?
Low-impact activities such as water aerobics, stationary biking, and stretching exercises are beneficial. Strengthening the quadriceps is particularly helpful.
Osteoarthritis of the knee is a prevalent, progressive condition requiring a strategic, multi-disciplinary approach for optimal management. Early diagnosis, patient education, weight control, structured physical therapy, and judicious use of pharmacologic or surgical interventions are essential to preserving mobility and function. Through personalized care plans, we can mitigate symptoms, delay progression, and enhance the quality of life for individuals living with knee OA.