organophosphorus overdose: Organophosphorous (OP) compounds, widely used in agriculture as pesticides, pose significant health hazards when ingested, inhaled, or absorbed in excessive amounts. An organophosphorous overdose results in the inhibition of acetylcholinesterase (AChE), causing an accumulation of acetylcholine at synaptic junctions. This leads to acute cholinergic toxicity, which can rapidly become fatal without timely intervention.
Overdose commonly occurs due to intentional ingestion in suicide attempts, occupational exposure, or accidental contact in agricultural or domestic settings.
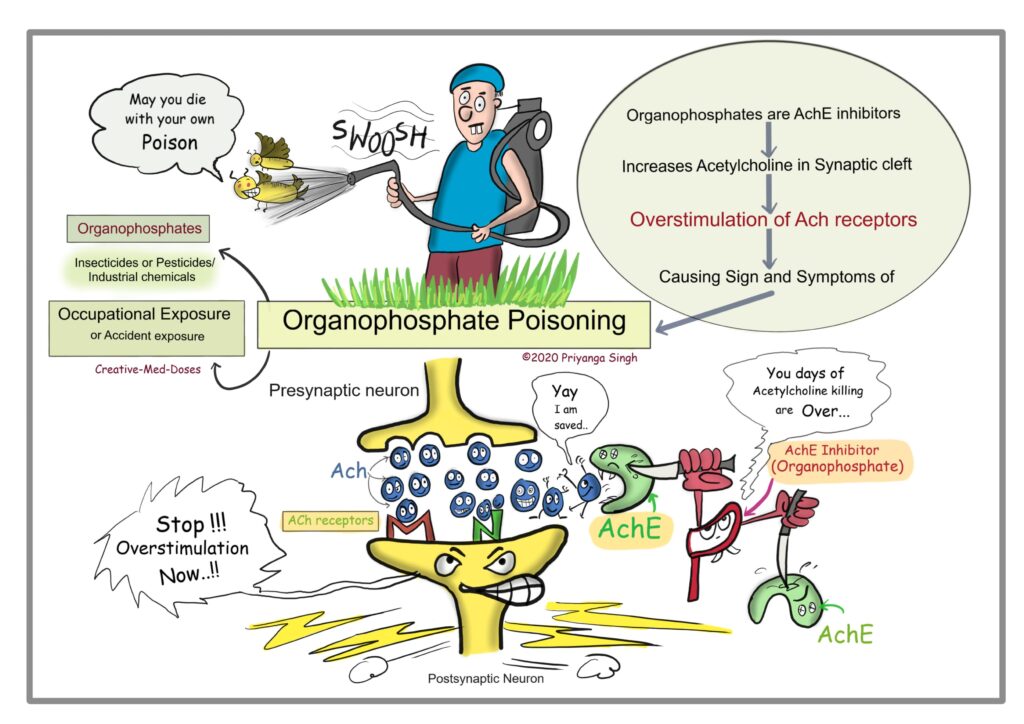
Pathophysiology: Acetylcholinesterase Inhibition and Cholinergic Overdrive
OP compounds bind irreversibly to acetylcholinesterase, impairing its ability to break down acetylcholine. The surplus acetylcholine overstimulates muscarinic, nicotinic, and central nervous system receptors.
Routes and Sources of Exposure on organophosphorus overdose
- Ingestion: Most common in self-harm cases
- Inhalation: From spraying in poorly ventilated areas
- Dermal absorption: Especially through broken skin
- Occupational hazard: Farm workers, pest control professionals
Common OP compounds include malathion, parathion, chlorpyrifos, diazinon, and phorate.
Clinical Features of Organophosphorous Overdose
Muscarinic Symptoms (Parasympathetic Overactivity)
- Salivation
- Lacrimation
- Urination
- Diarrhea
- Gastrointestinal cramps
- Emesis
- Bronchorrhea, bronchospasm
- Miosis (constricted pupils)
- Bradycardia, hypotension
(Mnemonic: SLUDGE/BBB)
Nicotinic Symptoms (Neuromuscular Effects)
- Muscle fasciculations
- Twitching
- Cramping
- Paralysis
- Tachycardia
- Hypertension
Central Nervous System Effects
- Restlessness
- Anxiety
- Confusion
- Seizures
- Coma
- Respiratory depression
Diagnostic Approach to Organophosphorous Overdose
Clinical Diagnosis
Diagnosis is primarily clinical, based on:
- Sudden onset of cholinergic symptoms
- History of exposure to pesticides
- Characteristic garlic-like odor
Laboratory Investigations
- Plasma pseudocholinesterase: Rapidly falls after exposure
- RBC acetylcholinesterase: More specific, correlates with severity
- ABG: For respiratory acidosis
- ECG: To monitor cardiac arrhythmias
- Chest X-ray: For aspiration pneumonia or pulmonary edema
- Serum electrolytes, renal, and hepatic panels
Emergency Management of Organophosphorous Overdose
Initial Stabilization
- Airway: Secure and maintain; intubate if needed
- Breathing: Administer oxygen; ventilate if respiratory distress is present
- Circulation: IV fluids for hypotension; monitor cardiac rhythm
Decontamination
- Remove contaminated clothing
- Irrigate skin and mucous membranes with water
- Activated charcoal if ingestion is recent and airway is secure
Antidotal Treatment
Atropine
- Mechanism: Blocks muscarinic receptors
- Initial dose: 1–2 mg IV every 5–10 minutes
- Titrated until: Lungs are dry, pulse ≥80 bpm, blood pressure normalizes
- High doses (hundreds of mg) may be required
Oximes (Pralidoxime or Obidoxime)
- Mechanism: Reactivates acetylcholinesterase before “aging” occurs
- Loading dose: 30 mg/kg IV over 30 minutes
- Maintenance: Continuous infusion or repeated boluses
- Best used early within 24–48 hours post-exposure
Seizure Control
- Diazepam or lorazepam IV for CNS excitation
Intermediate Syndrome and Delayed Effects
Intermediate Syndrome
- Occurs 1–4 days after apparent recovery
- Characterized by:
- Neck muscle weakness
- Proximal limb weakness
- Respiratory insufficiency
- Requires mechanical ventilation for several days
Organophosphate-Induced Delayed Neuropathy (OPIDN)
- Presents 1–3 weeks post-exposure
- Progressive sensory-motor polyneuropathy
- Primarily affects lower limbs
- May persist for months to years
- Management is supportive and includes physiotherapy
Prognosis and Complications
Prognostic Factors
- Amount and type of OP compound ingested
- Time elapsed before treatment
- Level of enzyme inhibition
- Presence of complications like aspiration or seizures
Common Complications
- Respiratory failure
- Sepsis from aspiration pneumonia
- Cardiac arrhythmias
- Persistent vegetative state after prolonged coma
Mortality can range from 5–40%, with higher rates in delayed or improperly managed cases.
Prevention and Public Health Implications
Individual-Level Precautions
- Proper handling and use of PPE
- Never store pesticides in food or drink containers
- Educate at-risk populations about safe usage and disposal
Regulatory and Policy Measures
- Restrict access to highly toxic OP compounds
- Promote alternative pest control strategies (IPM)
- Train healthcare providers in early recognition and treatment
- Implement poison control centers with access to antidotes
Frequently Asked Questions: organophosphorus overdose
What is the most important initial step in OP overdose?
Securing the airway and initiating atropine therapy to manage muscarinic symptoms.
How quickly should pralidoxime be administered?
Ideally within the first 24–48 hours to maximize efficacy before the AChE-OP complex “ages.”
What are the signs of atropine toxicity?
Dry mouth, blurred vision, tachycardia, and confusion indicate atropine overdose.
Can OP overdose cause long-term effects?
Yes. Delayed neuropathy and cognitive impairment may persist for months to years.
Are all insecticides organophosphates?
No. Other classes include carbamates and pyrethroids, which differ in toxicity and treatment.
Organophosphorous overdose remains a critical toxicological emergency worldwide, particularly in low-resource and agricultural settings. A thorough understanding of the clinical features, rapid recognition of cholinergic toxicity, and aggressive intervention using atropine and oximes are central to reducing mortality. Long-term rehabilitation and prevention strategies are crucial to minimize the burden of OP poisoning and improve patient outcomes.