Organ transplant rejection is a complex immunological response wherein the recipient’s immune system identifies the transplanted organ as foreign and mounts an attack against it. Despite advancements in surgical techniques and immunosuppressive therapy, rejection remains a significant challenge to transplant success and long-term graft survival.
Understanding the types, underlying mechanisms, early detection, and strategies for prevention is essential in optimizing outcomes for transplant recipients.
Types of Organ Transplant Rejection
Transplant rejection can be classified based on the timing and immune mechanisms involved.
Hyperacute Rejection
- Onset: Minutes to hours post-transplant
- Cause: Pre-existing antibodies against donor antigens
- Mechanism: Antibody-mediated damage leading to rapid thrombosis and graft necrosis
- Outcome: Irreversible; requires immediate removal of the graft
Acute Rejection
- Onset: Days to months after transplant
- Types:
- Cellular (T-cell mediated rejection, TCMR): Characterized by T lymphocyte infiltration
- Humoral (Antibody-mediated rejection, AMR): Caused by donor-specific antibodies (DSAs)
- Symptoms: Fever, graft tenderness, declining organ function
- Treatment: High-dose corticosteroids, anti-thymocyte globulin, plasmapheresis
Chronic Rejection
- Onset: Months to years post-transplant
- Mechanism: Progressive vascular injury, fibrosis, and organ dysfunction
- Common in: Heart (cardiac allograft vasculopathy), kidney (interstitial fibrosis and tubular atrophy), lung (bronchiolitis obliterans)
- Management: Limited; focus on slowing progression with immunomodulators
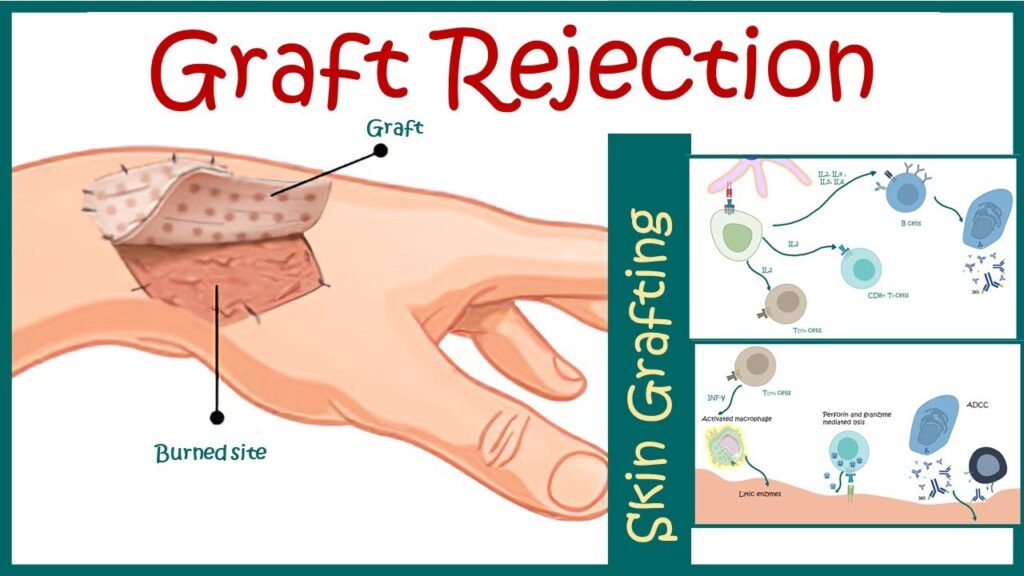
Pathophysiology of Transplant Rejection
Organ rejection is primarily driven by the recognition of donor antigens by the recipient’s immune system, initiating a cascade of inflammatory and cytotoxic responses.
This immune cascade results in varying degrees of graft injury depending on the type of immune response elicited.
Risk Factors for Transplant Rejection
- HLA mismatch between donor and recipient
- Sensitization from previous transplants, transfusions, or pregnancies
- Inadequate immunosuppression
- Infections triggering immune activation
- Non-adherence to prescribed medications
- Younger age of recipient (more robust immune response)
Identification and mitigation of these risk factors are essential during the pre-transplant evaluation.
Clinical Signs and Symptoms of Rejection
Rejection can be asymptomatic in early stages, making routine surveillance crucial. Common manifestations by organ type include:
Kidney Transplant
- Rising serum creatinine
- Decreased urine output
- Hypertension
- Graft tenderness
Heart Transplant
- Fatigue
- Arrhythmias
- Shortness of breath
- Reduced ejection fraction on echocardiography
Liver Transplant
- Jaundice
- Elevated liver enzymes (AST, ALT, ALP)
- Right upper quadrant pain
Lung Transplant
- Decline in pulmonary function tests
- Dyspnea
- Persistent cough
Diagnostic Tools for Detecting Rejection
Laboratory Tests
- Serum creatinine, liver enzymes, cardiac biomarkers
- Donor-specific antibody (DSA) testing
- Complete blood count and inflammatory markers
Imaging
- Ultrasound or Doppler for renal graft perfusion
- Echocardiography for cardiac function
- Chest X-ray or CT scan for lung assessment
Biopsy (Gold Standard)
- Histological analysis of graft tissue
- Banff classification (for kidney)
- ISHLT grading (for heart)
Biopsy remains the most definitive tool for characterizing rejection type and severity.
Immunosuppressive Therapy to Prevent Rejection
Immunosuppressive regimens aim to balance prevention of rejection with minimizing toxicity and infection risks.
Induction Therapy
- Given perioperatively to prevent early rejection
- Agents: Basiliximab, antithymocyte globulin, alemtuzumab
Maintenance Therapy
- Long-term regimen typically includes:
- Calcineurin inhibitors (CNI): Tacrolimus or cyclosporine
- Antimetabolites: Mycophenolate mofetil or azathioprine
- Corticosteroids: Prednisone
- mTOR inhibitors (optional): Sirolimus, everolimus
Close therapeutic drug monitoring is critical to avoid under- or over-immunosuppression.
Managing Acute and Chronic Rejection
Acute Rejection
- Corticosteroids: First-line for mild-moderate TCMR
- Anti-thymocyte globulin: Severe or steroid-resistant cases
- Plasmapheresis + IVIG: For AMR with high DSA levels
- Rituximab/Eculizumab: Targeted B-cell and complement inhibition
Chronic Rejection
- Difficult to reverse; management includes:
- Optimizing immunosuppression
- Treating comorbidities (hypertension, hyperlipidemia)
- Re-transplantation in selected cases
Monitoring and Long-Term Follow-up
Lifelong surveillance is imperative to detect rejection early and preserve graft function.
Follow-up Protocol
- Routine blood tests: Renal/liver function, immunosuppressant levels
- DSA screening: At set intervals
- Protocol biopsies: In high-risk patients
- Adherence support: Medication compliance is vital
Patient education on signs of rejection, infection precautions, and regular clinic visits enhances long-term outcomes.
Emerging Therapies and Research
Innovative approaches are under investigation to reduce rejection rates and improve graft survival:
- Cell-based therapies: Regulatory T cells to induce tolerance
- Gene editing: CRISPR-modified donor organs with reduced immunogenicity
- Biomarkers: Non-invasive molecular markers to detect rejection
- Xenotransplantation: Genetically modified animal organs as future graft sources
These advancements may redefine transplant immunology and rejection management.
Frequently Asked Questions:
Can transplant rejection be completely prevented?
While the risk can be minimized through immunosuppression and HLA matching, complete prevention is not yet achievable.
How quickly can rejection occur after transplant?
Hyperacute rejection happens within hours, acute within weeks to months, and chronic over months to years.
Are all transplant patients at risk of rejection?
Yes. All recipients are at risk, but with different probabilities depending on organ type, genetic match, and immunosuppression.
Is biopsy always required to confirm rejection?
Yes, in most cases, biopsy is the gold standard to confirm and grade rejection.
Can a rejected organ be replaced?
Re-transplantation may be considered depending on the patient’s condition and eligibility.
Organ transplant rejection is a multifaceted immunological challenge that requires vigilant monitoring, tailored immunosuppressive strategies, and timely intervention. Recognizing the types of rejection, understanding the underlying mechanisms, and adhering to preventive measures can significantly enhance graft survival and patient quality of life. Continuous research and clinical advancements hold promise for reducing rejection rates and improving long-term transplant success.