Optic neuritis is an inflammatory condition affecting the optic nerve, the structure responsible for transmitting visual information from the eye to the brain. This condition often leads to sudden vision loss, eye pain, and color vision abnormalities. It is most commonly associated with multiple sclerosis (MS) but can also occur independently or in connection with other autoimmune, infectious, or neurological disorders. Early identification and management are vital to preserving visual function and detecting underlying systemic conditions.
Anatomy and Function of the Optic Nerve
The optic nerve, or cranial nerve II, comprises over one million nerve fibers originating from the retinal ganglion cells. It serves as the essential conduit between the retina and the visual cortex in the brain. Any disruption, especially through inflammation or demyelination, significantly impairs visual signal transmission.
Causes and Risk Factors of Optic Neuritis
Primary Causes
- Multiple Sclerosis (MS): Optic neuritis is frequently the first manifestation of MS, a chronic demyelinating disease of the central nervous system.
- Neuromyelitis Optica Spectrum Disorder (NMOSD): A severe demyelinating condition that can mimic MS but often presents with bilateral optic neuritis.
- Myelin Oligodendrocyte Glycoprotein Antibody Disease (MOGAD): Inflammatory disorder with recurrent optic neuritis episodes.
Secondary Causes
- Infectious agents: Herpes viruses, syphilis, Lyme disease, and tuberculosis.
- Autoimmune disorders: Lupus, sarcoidosis, Behçet’s disease.
- Medications and toxins: Ethambutol, methanol, or immune checkpoint inhibitors.
- Paraneoplastic syndromes associated with malignancies.
Symptoms of Optic Neuritis: Clinical Presentation
The typical presentation of optic neuritis includes:
- Sudden, unilateral vision loss (occasionally bilateral in children or NMOSD)
- Ocular pain, especially during eye movement
- Decreased color perception, particularly for red hues (red desaturation)
- Visual field defects, such as central scotomas
- Relative afferent pupillary defect (RAPD) on affected side
- Phosphenes (flashes of light with eye movement)
Vision loss generally progresses over hours to days, often peaking within one week.
Diagnosis of Optic Neuritis: Evaluating the Underlying Cause
Clinical Assessment
- Ophthalmologic examination reveals reduced visual acuity, color vision defects, and visual field loss.
- Pupillary response testing shows a positive RAPD in unilateral cases.
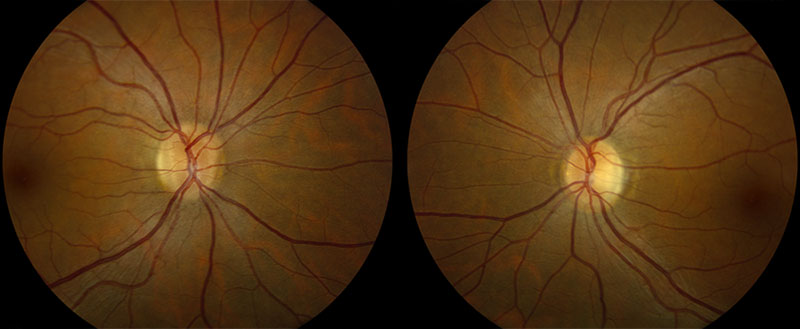
- Fundoscopy: The optic disc appears normal in retrobulbar neuritis but may show swelling (papillitis) in anterior neuritis.
Imaging and Laboratory Investigations
- MRI of the brain and orbits with contrast: Key to detecting optic nerve inflammation and identifying white matter lesions suggestive of MS.
- Lumbar puncture: CSF analysis for oligoclonal bands if MS or NMOSD is suspected.
- Serological tests: AQP4-IgG and MOG-IgG antibodies help differentiate between NMOSD and MOGAD.
- Visual evoked potentials (VEP): Assesses the speed of visual signal transmission, often delayed in demyelinating diseases.
Optic Neuritis and Multiple Sclerosis: A Diagnostic Nexus
Approximately 50% of individuals with MS will experience optic neuritis during the course of their disease, and 20% of MS cases initially present with optic neuritis. The risk of developing MS after a first episode of optic neuritis increases significantly when MRI lesions characteristic of MS are present. Longitudinal monitoring with neurologic evaluations and repeat imaging is essential in such patients.
Treatment Options for Optic Neuritis
Acute Management
- High-dose intravenous corticosteroids (methylprednisolone 1g/day for 3–5 days) are the standard treatment.
- Shortens recovery time
- Does not improve long-term visual outcomes or reduce risk of MS
- Oral steroids alone are not recommended due to higher relapse rates.
Additional Therapies
- Plasma exchange (PLEX): Considered in severe or steroid-refractory cases, especially in NMOSD.
- Disease-modifying therapies (DMTs): Initiated if MS or related disorders are diagnosed, to reduce relapse risk.
Prognosis and Long-Term Outcomes
Favorable Outlook
- Most patients with demyelinating optic neuritis regain 20/40 vision or better within six months.
- Visual recovery often begins within two weeks post-treatment.
Risk of Recurrence
- Higher in patients with MOG antibody-associated disease
- Recurrent episodes may lead to permanent vision impairment
Unfavorable Indicators
- Bilateral onset
- Poor initial visual acuity
- NMOSD-related optic neuritis
- Absence of recovery within one month
Differential Diagnosis: Conditions Mimicking Optic Neuritis
- Ischemic optic neuropathy – typically in older adults, with sudden painless vision loss
- Leber hereditary optic neuropathy (LHON) – mitochondrial disorder causing painless bilateral vision loss in young males
- Compressive optic neuropathy – due to tumors or orbital masses
- Toxic/nutritional optic neuropathy – due to alcohol, tobacco, B12 deficiency
Careful evaluation of symptoms, imaging, and blood tests are necessary to rule out these possibilities.
Preventive Strategies and Patient Education
- Avoid unproven alternative therapies that may delay diagnosis.
- Educate patients on the importance of follow-up to monitor for MS development.
- Lifestyle adjustments for those with demyelinating disease, including vitamin D optimization and smoking cessation.
Optic neuritis is a clinically significant condition that serves both as a standalone diagnosis and a potential harbinger of central nervous system demyelinating diseases such as multiple sclerosis. Prompt recognition, accurate diagnosis, and targeted treatment are critical to preserving visual function and managing long-term neurologic health. A multidisciplinary approach, involving neurology and ophthalmology, ensures optimal patient outcomes and reduces recurrence risks.