Bilateral anorchia, often referred to as “vanishing testes syndrome,” is a rare medical condition characterized by the absence of both testes at birth or their subsequent disappearance during early development. This article provides an in-depth look at the condition, covering its causes, symptoms, diagnosis, treatment options, and prognosis.
Understanding Bilateral Anorchia
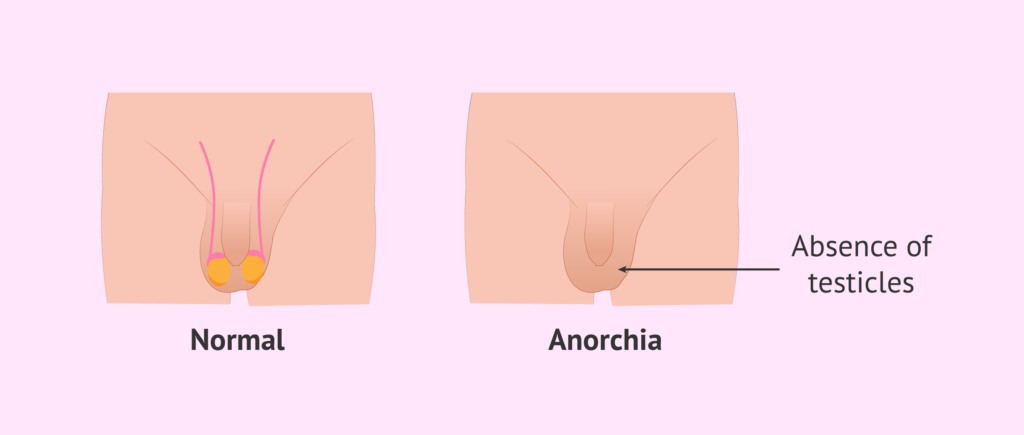
Bilateral anorchia is a congenital condition in which both testes are absent. The condition may arise during fetal development, often linked to interrupted or abnormal testicular formation after the initial differentiation of male genitalia. Despite the absence of testes, affected individuals typically have a 46,XY karyotype and external male genitalia.
Causes of Bilateral Anorchia
The exact cause of bilateral anorchia is not always clear, but several factors may contribute:
- Genetic mutations: Variants in specific genes like SRY or NR5A1 may disrupt normal testicular development.
- Vascular accidents: Testicular regression syndrome (TRS) may result from torsion or impaired blood flow during fetal development.
- Hormonal disruptions: Deficiencies in gonadotropins or androgen insensitivity can hinder testicular formation.
Recognizing the Symptoms
Symptoms vary depending on the timing of testicular regression. Key signs include:
- Neonatal phase: Normal male genitalia without palpable testes in the scrotum.
- Childhood: Delayed or absent secondary sexual characteristics such as lack of voice deepening, pubic hair, or growth spurts during puberty.
- Infertility: In adult patients, infertility is common due to the absence of sperm production.
Diagnostic Approach
Clinical Evaluation
A thorough medical history and physical examination are the first steps in diagnosing bilateral anorchia. Physicians will look for:
- Non-palpable testes in the scrotum or inguinal region.
- Normal penile length and male external genitalia.
Laboratory Tests
- Hormonal profiling: Low levels of testosterone, along with elevated luteinizing hormone (LH) and follicle-stimulating hormone (FSH), suggest primary testicular failure.
- Karyotyping: Confirms the presence of a 46,XY genotype.
- Anti-Müllerian hormone (AMH): Undetectable or low levels support the diagnosis of testicular absence.
Imaging Studies
Ultrasound and magnetic resonance imaging (MRI) are employed to locate any remnants of testicular tissue or to rule out cryptorchidism.
Surgical Exploration
In some cases, laparoscopy or open surgery is necessary to confirm the absence of testicular tissue and assess any remnants.
Treatment Options
Hormone Replacement Therapy (HRT)
The cornerstone of treatment is hormone replacement therapy to induce and maintain secondary sexual characteristics. Testosterone is commonly administered through:
- Injections
- Transdermal patches
- Gels
Psychological Support
Psychological counseling is crucial to address issues related to body image, identity, and infertility.
Fertility Considerations
While natural fertility is not possible, options such as sperm donation or adoption can be explored.
Prognosis and Long-Term Outcomes
With appropriate medical and psychological support, individuals with bilateral anorchia can lead fulfilling lives. Early diagnosis and treatment are critical to minimizing complications related to delayed puberty and low bone density.
Frequently Asked Questions
Can bilateral anorchia be prevented?
Currently, there are no known preventive measures due to the complex and often unknown causes of the condition.
Is bilateral anorchia hereditary?
In some cases, genetic factors play a role, but most instances appear sporadic without a familial pattern.
What is the life expectancy for individuals with bilateral anorchia?
Life expectancy is generally unaffected, provided that hormone therapy and medical care are properly managed.