Bacteroides endocarditis, a rare but severe form of bacterial endocarditis, arises from the infection of heart valves or the endocardium by Bacteroides species. This anaerobic Gram-negative bacteria, typically part of the human gut microbiota, can become pathogenic under specific conditions, leading to life-threatening complications. This article delves into its causes, clinical presentation, diagnostic approaches, and treatment options to provide a detailed understanding.
What is Bacteroides Endocarditis?
Bacteroides endocarditis is an infection of the inner lining of the heart or its valves caused predominantly by Bacteroides fragilis, among other Bacteroides species. These bacteria are obligate anaerobes and are generally non-invasive. However, in cases of disrupted mucosal barriers, such as gastrointestinal or surgical breaches, they can translocate into the bloodstream and establish an infection within the heart.
Causes and Risk Factors
Primary Causes
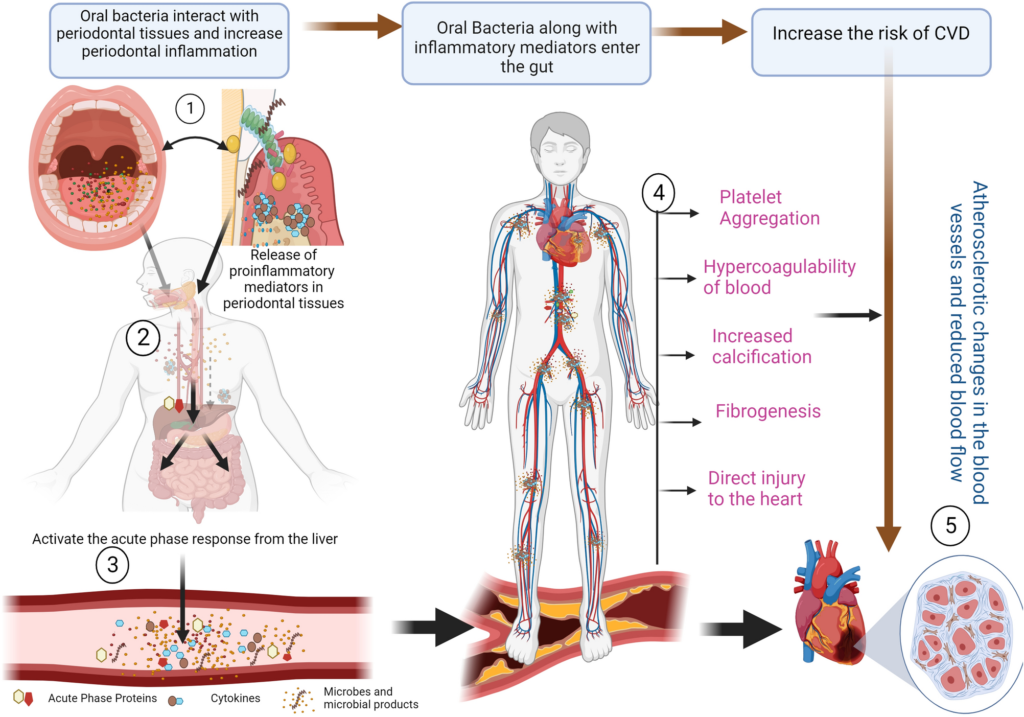
- Invasive Medical Procedures: Gastrointestinal surgeries or dental procedures can introduce Bacteroides into the bloodstream.
- Mucosal Injury: Conditions like diverticulitis or inflammatory bowel disease (IBD) can compromise the gut lining.
- Trauma: Abdominal trauma can disrupt mucosal barriers, allowing bacterial entry.
Risk Factors
- Prosthetic Heart Valves: Increased susceptibility due to foreign material.
- Congenital Heart Defects: Structural abnormalities favor bacterial colonization.
- Immunosuppression: Conditions such as HIV, diabetes, or immunosuppressive therapy weaken defenses.
- Previous Endocarditis: Prior infection increases the likelihood of recurrence.
Clinical Presentation
Bacteroides endocarditis often presents with nonspecific symptoms, complicating early diagnosis. Symptoms may include:
- Fever: Persistent or intermittent fever is common.
- Murmurs: New or changing cardiac murmurs signal valvular involvement.
- Fatigue: Generalized malaise and lethargy.
- Weight Loss: Unintentional weight loss due to systemic infection.
- Embolic Phenomena: Embolization to organs may cause symptoms like stroke or limb ischemia.
Diagnostic Approaches
Blood Cultures
Repeated blood cultures are critical for identifying Bacteroides species. Anaerobic culture techniques are necessary to isolate these bacteria.
Echocardiography
- Transthoracic Echocardiography (TTE): Initial imaging modality to detect vegetations.
- Transesophageal Echocardiography (TEE): Superior sensitivity for detecting smaller vegetations and abscesses.
Laboratory Findings
- Elevated inflammatory markers: C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR).
- Anemia of chronic disease.
Advanced Techniques
- PCR and Molecular Testing: Detect bacterial DNA for faster and more accurate identification.
- Histopathology: Examination of excised valve tissue confirms the diagnosis.
Treatment Options
Antibiotic Therapy
The cornerstone of treatment is prolonged antibiotic therapy targeting anaerobic bacteria. Common regimens include:
- Beta-lactams: Piperacillin-tazobactam or carbapenems.
- Metronidazole: Effective against anaerobes.
- Combination Therapy: To cover polymicrobial infections often associated with Bacteroides endocarditis.
Duration: 4-6 weeks of intravenous antibiotics.
Surgical Intervention
Indicated in cases of:
- Refractory infection despite antibiotics.
- Large vegetations causing embolization.
- Structural damage to heart valves.
Adjunctive Measures
- Supportive Care: Antipyretics, fluids, and hemodynamic stabilization.
- Monitoring for Complications: Surveillance for septic emboli or heart failure.
Prevention Strategies
Prophylactic Antibiotics
Patients at high risk, such as those with prosthetic valves or prior endocarditis, should receive prophylactic antibiotics before invasive procedures.
Managing Underlying Conditions
Effective control of gastrointestinal disorders or other risk factors reduces the likelihood of bacteremia.
Prognosis
Early diagnosis and treatment significantly improve outcomes. However, delayed treatment or complications like septic emboli can worsen the prognosis. Surgical intervention, when necessary, further enhances survival rates.