Non-infectious uveitis affecting the posterior segment of the eye is a serious inflammatory condition that involves the choroid, retina, and vitreous humor. Unlike infectious uveitis, it is not caused by microbial agents but rather by autoimmune and autoinflammatory mechanisms. This sight-threatening condition demands prompt diagnosis and long-term management due to its potential to cause irreversible vision loss.

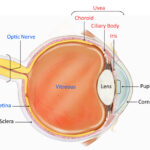
Anatomical Classification of Uveitis
Uveitis is categorized based on the primary site of inflammation:
- Anterior uveitis: Affects the iris and anterior chamber.
- Intermediate uveitis: Involves the vitreous and peripheral retina.
- Posterior uveitis: Affects the retina and choroid.
- Panuveitis: Involves all segments of the uvea.
Non-infectious posterior uveitis specifically refers to immune-mediated inflammation isolated to the retina and/or choroid.
Etiology: Underlying Causes and Associated Conditions
Non-infectious posterior uveitis often arises from systemic autoimmune diseases or as an isolated idiopathic condition. Key etiologies include:
- Behçet’s disease
- Sarcoidosis
- Vogt-Koyanagi-Harada (VKH) syndrome
- Multiple sclerosis
- Systemic lupus erythematosus
- Sympathetic ophthalmia
- Birdshot chorioretinopathy
In these diseases, immune dysregulation leads to inflammation of ocular structures, primarily targeting retinal vessels, the retinal pigment epithelium (RPE), and the choroid.
Clinical Presentation: Symptoms of Posterior Segment Uveitis
Symptoms are typically insidious in onset and may vary depending on the affected structures. Common manifestations include:
- Blurred or decreased vision
- Floaters
- Photopsia (light flashes)
- Scotomas (visual field defects)
- Eye discomfort or mild redness (less common than in anterior uveitis)
Severe or chronic inflammation may lead to complications such as cystoid macular edema, retinal vasculitis, choroidal neovascularization, and optic disc edema.
Diagnostic Evaluation of Non-Infectious Posterior Uveitis
A thorough diagnostic workup is essential to confirm the diagnosis and rule out infectious or malignant mimics.
Clinical Examination
- Fundus examination reveals retinal infiltrates, vasculitis, choroiditis, or vitreous haze.
- Use of slit-lamp biomicroscopy with indirect ophthalmoscopy.
Imaging Studies
- Optical Coherence Tomography (OCT): Detects macular edema and subretinal fluid.
- Fluorescein Angiography (FA): Evaluates retinal vascular leakage.
- Indocyanine Green Angiography (ICGA): Assesses choroidal circulation.
- Fundus autofluorescence (FAF): Highlights RPE damage.
Laboratory Testing
To determine systemic associations:
- ACE levels, ANA, HLA typing, ESR/CRP
- Chest X-ray or CT for sarcoidosis
- MRI for CNS involvement (e.g., in MS)
Exclusion of Infections
Serologies and PCR testing may be performed to rule out toxoplasmosis, tuberculosis, syphilis, and viral etiologies, even in presumed non-infectious cases.
Treatment Strategies for Non-Infectious Posterior Uveitis
Effective management depends on controlling inflammation and preventing relapses, while minimizing long-term complications and treatment side effects.
1. Corticosteroids
- First-line treatment due to potent anti-inflammatory effects.
- Delivered via systemic (oral or IV), periocular, or intravitreal routes.
- Long-term use is limited by systemic side effects like osteoporosis, hypertension, and cataracts.
2. Immunomodulatory Therapy (IMT)
Indicated in steroid-resistant or recurrent cases.
- Methotrexate, azathioprine, mycophenolate mofetil for maintenance therapy.
- Requires regular blood monitoring to assess liver, kidney, and blood counts.
3. Biologic Agents
Biologics target specific immune pathways.
- Anti-TNF-α agents (e.g., adalimumab, infliximab) for Behçet’s disease or refractory uveitis.
- Interleukin inhibitors and B-cell targeted therapy (rituximab) are under investigation or used in complex cases.
4. Local Steroid Implants
- Dexamethasone intravitreal implant (Ozurdex)
- Fluocinolone acetonide implant (Retisert, Yutiq)
Provide long-acting control with reduced systemic exposure but may induce cataract or glaucoma.
5. Adjunctive Therapies
- Cycloplegics to relieve ciliary spasm.
- Antiglaucoma medications if intraocular pressure is elevated.
- Management of complications like macular edema using anti-VEGF agents or laser therapy.
Prognosis and Long-Term Monitoring
The visual prognosis depends on:
- Prompt diagnosis
- Effective suppression of inflammation
- Early management of complications
Patients require regular follow-ups to monitor for disease recurrence, ocular side effects of therapy, and systemic disease progression.
Emerging Therapies and Future Directions
Advancements in immunology have led to:
- Targeted biologics with higher specificity
- Gene expression profiling for personalized treatment
- Sustained-release drug delivery systems
Clinical trials continue to refine therapeutic regimens, aiming to reduce systemic immunosuppression and maintain long-term ocular remission.
Non-infectious uveitis affecting the posterior segment of the eye represents a complex interplay of ocular and systemic inflammation. Accurate diagnosis, multidisciplinary collaboration, and individualized treatment plans are essential to preserving vision. With the advent of biologic therapies and imaging innovations, outcomes for patients with posterior uveitis have significantly improved, offering a promising future in the management of this potentially blinding condition.