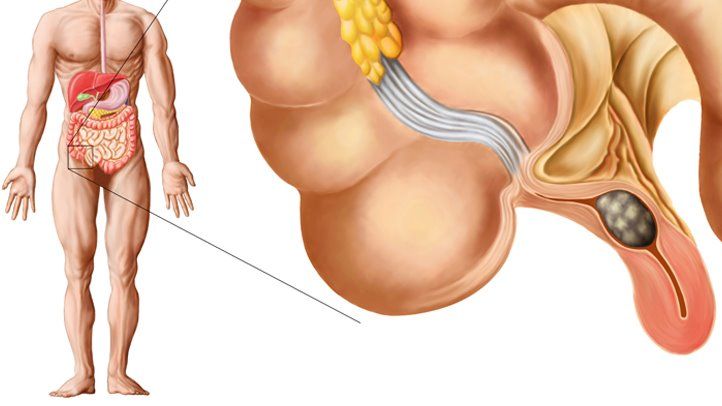
Appendicitis, one of the most common acute abdominal conditions requiring surgical intervention, has been increasingly studied for its microbial involvement. Among the various bacterial species identified in the inflamed appendix, Bacteroides stands out as a key player in the pathogenesis of appendicitis. This article delves into the relationship between Bacteroides and appendicitis, exploring its role in the onset, progression, and treatment of this condition.
What is Appendicitis?
Appendicitis is the inflammation of the appendix, a small, tube-like structure attached to the large intestine. The condition typically presents as acute abdominal pain, nausea, vomiting, and fever. If left untreated, it can lead to severe complications, including perforation, peritonitis, and sepsis. Appendectomy, the surgical removal of the appendix, is the standard treatment for acute appendicitis.
Bacteroides and Its Role in Appendicitis
Bacteroides is a genus of Gram-negative, obligate anaerobic bacteria that are a normal part of the human gut microbiota. These bacteria are involved in the breakdown of complex molecules, particularly in the colon. Although Bacteroides species are usually harmless, their overgrowth or translocation to other parts of the body can lead to infections.
Recent studies have highlighted the role of Bacteroides in the pathogenesis of appendicitis. It is believed that Bacteroides bacteria, particularly Bacteroides fragilis, are frequently involved in the early stages of the condition. When the appendix becomes obstructed, typically by fecal matter, lymphoid hyperplasia, or a foreign body, the anaerobic environment inside the appendix allows Bacteroides species to proliferate. This proliferation leads to the release of toxins and inflammatory mediators that contribute to the acute inflammatory response characteristic of appendicitis.
The Mechanism Behind Bacteroides-Induced Appendicitis
The obstruction of the appendix creates an ideal environment for Bacteroides to thrive. The lack of oxygen in the closed-off appendix favors anaerobic bacteria, including Bacteroides fragilis, Bacteroides vulgatus, and Bacteroides thetaiotaomicron. These bacteria are part of the normal flora but can become pathogenic when the appendix is compromised.
Once the bacteria multiply, they initiate an inflammatory cascade that results in the swelling and pain associated with appendicitis. The release of bacterial endotoxins and other virulence factors exacerbates the immune response, leading to tissue damage and pus formation within the appendix. In severe cases, the infection may spread to the peritoneal cavity, leading to peritonitis, a life-threatening complication.
The Role of Bacteroides in Complicated Appendicitis
While uncomplicated appendicitis can usually be managed with antibiotics and appendectomy, the presence of Bacteroides species is linked to more complicated forms of the condition. Studies have shown that Bacteroides is commonly found in the microbiota of patients with perforated appendicitis, indicating that the bacterial load and type of microbiota present may influence the severity of the disease.
Infected appendices containing high concentrations of Bacteroides are more prone to perforation due to the aggressive nature of these bacteria. The ability of Bacteroides to form biofilms, which are protective layers of bacterial cells, makes it even more difficult to treat infections involving these organisms. As a result, patients with complicated appendicitis may require prolonged antibiotic therapy to eradicate the infection and prevent further complications.
Diagnosis of Appendicitis Involving Bacteroides
Diagnosing appendicitis traditionally involves clinical evaluation, blood tests, and imaging techniques such as ultrasound or CT scans. However, with the increasing recognition of the role of Bacteroides in appendicitis, microbiological culture and molecular diagnostics are becoming more relevant.
Microbiological cultures from peritoneal fluid or appendiceal tissue samples can reveal the presence of Bacteroides species, confirming their involvement in the infection. Additionally, advanced molecular techniques, such as polymerase chain reaction (PCR) and 16S ribosomal RNA gene sequencing, can help identify specific Bacteroides species and determine their relative abundance in the infected appendix. These methods provide valuable insight into the microbial landscape of appendicitis and may help guide more effective treatment strategies.
Treatment of Appendicitis: The Role of Antibiotics
The management of appendicitis traditionally focuses on surgical intervention, specifically appendectomy, which remains the most effective treatment for acute appendicitis. However, antibiotics play a crucial role in the management of the infection, especially when Bacteroides species are involved.
Antibiotics for Appendicitis Involving Bacteroides
Empiric antibiotic therapy typically includes broad-spectrum antibiotics that cover both Gram-negative and anaerobic bacteria. Bacteroides species are often resistant to certain antibiotics, making them a challenge to treat. Therefore, antibiotics such as piperacillin-tazobactam, meropenem, or metronidazole are commonly used to target Bacteroides and other anaerobic pathogens.
In cases of complicated appendicitis, where there is a high risk of perforation or abscess formation, prolonged or adjusted antibiotic therapy may be required. Additionally, postoperative antibiotic courses are recommended to prevent secondary infections and reduce the risk of sepsis.
Antibiotic Resistance and Bacteroides
A growing concern in the treatment of appendicitis is the development of antibiotic resistance, particularly among Bacteroides species. Overuse and misuse of antibiotics have led to the emergence of resistant strains, which complicates the treatment of appendicitis. As a result, research into alternative treatment options, including bacteriophage therapy and probiotics, is gaining momentum.
Preventing Appendicitis and Managing Gut Microbiota
The involvement of Bacteroides in appendicitis underscores the importance of maintaining a healthy gut microbiota. Dysbiosis, or an imbalance in the gut microbiome, can contribute to the overgrowth of pathogenic bacteria, including Bacteroides. A balanced diet rich in fiber and low in processed foods is essential for sustaining a healthy microbiome, potentially reducing the risk of appendicitis.
While genetic predisposition and environmental factors play significant roles in the development of appendicitis, interventions aimed at restoring microbiota balance may offer novel strategies for prevention. Probiotics and prebiotics, which promote the growth of beneficial bacteria, are being explored for their potential to prevent or mitigate the severity of appendicitis, particularly in individuals with a history of recurrent episodes.