Bacterial vaginosis (BV) is one of the most common vaginal infections, affecting a significant number of women worldwide. Despite its high prevalence, there is often confusion about the condition, including its causes, symptoms, treatment, and ways to prevent it. In this guide, we will explore everything you need to know about BV, providing clear insights into its nature and offering actionable advice for effective management and prevention.
What is Bacterial Vaginosis (BV)?
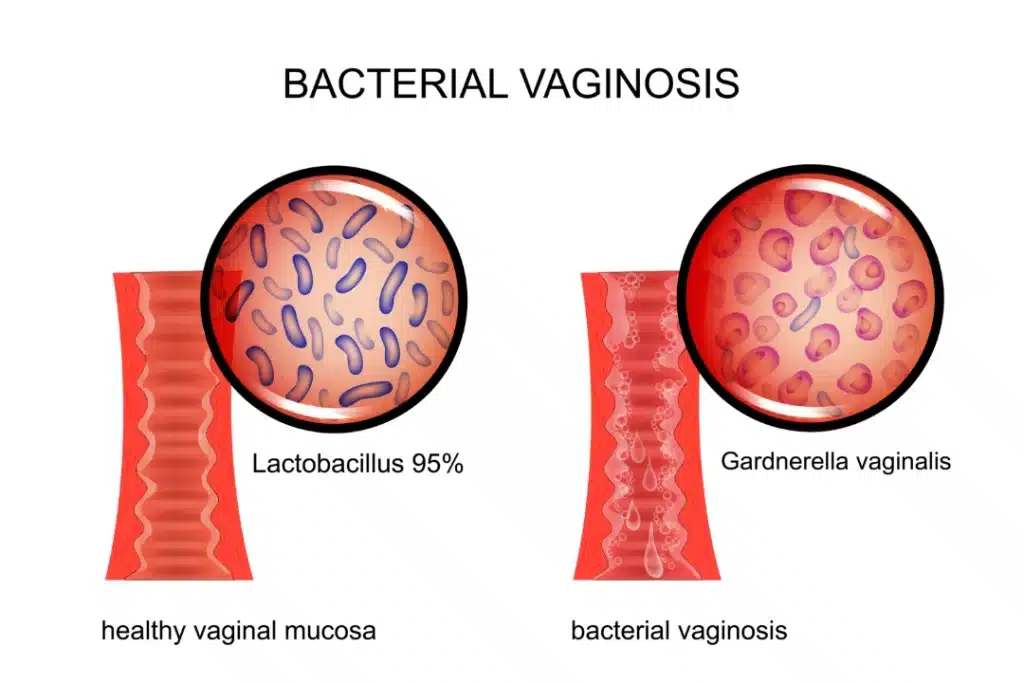
Bacterial vaginosis is an imbalance in the natural bacterial flora of the vagina. In a healthy vagina, a variety of bacteria live in harmony, predominantly Lactobacillus species, which help maintain an acidic environment that prevents the overgrowth of harmful bacteria. When there is a decrease in Lactobacilli and an increase in other types of bacteria, an infection can occur, leading to symptoms such as an unusual vaginal discharge and a fishy odor.
Unlike yeast infections, BV is caused by an overgrowth of bacteria rather than fungi, and it does not stem from sexual activity alone. It can affect women of all ages, whether sexually active or not.
Causes of Bacterial Vaginosis
The exact cause of BV is not fully understood, but several factors contribute to the development of this imbalance in vaginal flora. Common causes and risk factors include:
- Douching: Douching can disrupt the natural pH balance of the vagina, making it more susceptible to infections.
- Unprotected Sexual Activity: Although BV is not classified as a sexually transmitted infection (STI), new or multiple sexual partners can increase the risk.
- Antibiotic Use: Overuse of antibiotics can kill beneficial bacteria in the vagina, allowing harmful bacteria to proliferate.
- Hormonal Changes: Changes in hormone levels, particularly during pregnancy or menopause, can affect the vaginal environment.
- Intrauterine Devices (IUDs): Some studies suggest that the use of IUDs may increase the likelihood of developing BV.
By understanding these risk factors, individuals can take proactive steps to reduce their chances of developing BV.
Symptoms of Bacterial Vaginosis
The symptoms of BV can vary, but the most common include:
- Unusual Vaginal Discharge: A thin, gray, or white discharge that may have a strong, fishy odor, especially after intercourse.
- Vaginal Itching or Irritation: A feeling of discomfort or itching around the vaginal area.
- Pain During Urination: Some women with BV report a painful or burning sensation when urinating.
- Painful Intercourse: Pain during or after sexual activity may also be a symptom.
It’s important to note that some women with BV may not exhibit any symptoms at all. If left untreated, BV can lead to more serious complications, such as pelvic inflammatory disease (PID) or an increased risk of HIV transmission.
Diagnosing Bacterial Vaginosis
A healthcare provider typically diagnoses BV based on a physical examination, a review of symptoms, and laboratory tests. These tests may include:
- Vaginal pH Test: An increased pH level (above 4.5) in the vaginal discharge is indicative of BV.
- Microscopic Examination: A sample of vaginal discharge is examined under a microscope to check for the presence of “clue cells” (epithelial cells coated with bacteria).
- Whiff Test: A strong, fishy odor is detected when a drop of potassium hydroxide (KOH) is added to the vaginal discharge.
If you experience any symptoms of BV, it’s important to consult a healthcare professional for accurate diagnosis and treatment.
Treatment Options for Bacterial Vaginosis
Bacterial vaginosis is typically treated with antibiotics. The most common treatment options include:
- Metronidazole: This antibiotic is often prescribed in either oral or gel form. It is effective in eliminating the harmful bacteria that cause BV.
- Clindamycin: Available as a cream or oral medication, clindamycin is another effective treatment for BV.
It’s crucial to follow the prescribed treatment regimen completely to ensure the infection is fully treated. Failure to do so can lead to recurrence of the infection.
For women with recurrent BV, additional strategies may be recommended, such as:
- Probiotics: Taking probiotics, especially those containing Lactobacillus species, can help restore the natural balance of bacteria in the vagina.
- Maintaining Vaginal pH: Avoiding douching and using pH-balanced soaps may help prevent the recurrence of BV.
Preventing Bacterial Vaginosis
While bacterial vaginosis can’t always be prevented, there are several steps you can take to reduce your risk:
- Avoid Douching: Douching can disrupt the natural bacterial balance and should be avoided.
- Practice Safe Sex: Using condoms during sexual activity can reduce the risk of BV by minimizing exposure to bacteria.
- Wear Breathable Underwear: Cotton underwear allows for better ventilation, which helps maintain a healthy vaginal environment.
- Maintain Proper Hygiene: Gently wash the vaginal area with mild soap and water, avoiding harsh products or fragrances that can irritate the skin.
- Limit Antibiotic Use: Only use antibiotics when necessary, as overuse can lead to a disruption of the vaginal flora.
The Impact of Bacterial Vaginosis on Reproductive Health
Bacterial vaginosis can have implications for reproductive health, especially if left untreated. Women with BV are at an increased risk for certain complications, including:
- Pelvic Inflammatory Disease (PID): BV can increase the likelihood of developing PID, a serious infection of the reproductive organs.
- Preterm Birth: Pregnant women with BV are more likely to experience preterm birth or low birth weight.
- Increased Risk of HIV: Women with BV are at a higher risk of acquiring HIV if exposed to the virus.
For this reason, it’s important to address BV promptly and seek medical advice if you suspect you have the infection.
Natural Remedies for Bacterial Vaginosis
While medical treatments are essential for curing BV, some women seek natural remedies in addition to conventional therapies. Although the effectiveness of these remedies can vary, some options include:
- Garlic: Known for its antimicrobial properties, garlic may help reduce the bacterial imbalance in the vagina.
- Tea Tree Oil: This essential oil has been shown to possess antibacterial properties and may be beneficial when diluted and applied topically.
- Apple Cider Vinegar: Some women use diluted apple cider vinegar in a sitz bath to restore the vaginal pH.
It’s crucial to consult with a healthcare provider before trying natural remedies, especially if you’re already undergoing medical treatment.