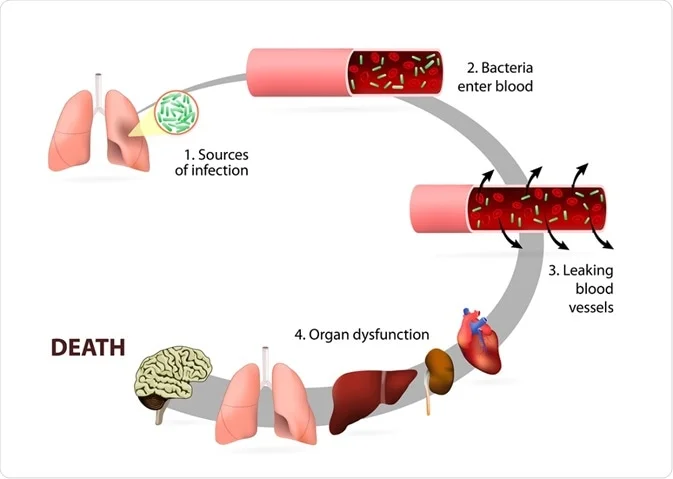
Bacterial sepsis is a life-threatening medical condition caused by the body’s extreme response to bacterial infection. This condition occurs when bacteria enter the bloodstream, triggering a chain reaction of inflammation and tissue damage that can lead to organ failure. Prompt diagnosis and treatment are crucial to improving survival rates.
What is Bacterial Sepsis?
Bacterial sepsis, commonly referred to as septicemia, is characterized by the presence of harmful bacteria in the bloodstream. It can escalate into septic shock, a severe state where blood pressure drops dangerously low, posing a significant risk to life. Understanding its pathophysiology is vital for timely intervention.
Key Features
- Systemic inflammation: Excessive immune response to bacterial invasion.
- Multi-organ dysfunction: Impaired organ function due to widespread inflammation.
- Potential for septic shock: Progression to critically low blood pressure.
Causes of Bacterial Sepsis
Bacterial sepsis originates from various infections, commonly affecting the respiratory system, urinary tract, abdominal cavity, or skin. Certain bacteria are more likely to cause sepsis, including:
- Gram-positive bacteria: Staphylococcus aureus, Streptococcus pneumoniae
- Gram-negative bacteria: Escherichia coli, Klebsiella pneumoniae, Pseudomonas aeruginosa
Risk factors include compromised immune systems, chronic diseases, invasive procedures, and prolonged hospital stays.
Symptoms of Bacterial Sepsis
Early recognition of bacterial sepsis is critical for effective treatment. Common symptoms include:
- Fever or hypothermia: Elevated or abnormally low body temperature.
- Tachycardia: Rapid heart rate.
- Tachypnea: Increased respiratory rate.
- Confusion: Altered mental state or disorientation.
- Hypotension: Low blood pressure in severe cases.
- Skin changes: Pale, clammy, or mottled skin.
Diagnosis of Bacterial Sepsis
Timely and accurate diagnosis is essential. Diagnostic measures include:
- Blood cultures: Identify bacterial presence and type.
- Laboratory tests: Assess inflammation markers like C-reactive protein (CRP) and procalcitonin.
- Imaging: CT scans or ultrasounds to locate infection sites.
- Clinical criteria: Based on Sequential Organ Failure Assessment (SOFA) or Quick SOFA (qSOFA) scores.
Treatment
Management of bacterial sepsis involves prompt and aggressive intervention to halt disease progression.
1. Antibiotic Therapy
Administer broad-spectrum antibiotics immediately, followed by targeted therapy based on culture results.
2. Fluid Resuscitation
Intravenous fluids stabilize blood pressure and improve circulation.
3. Vasoactive Medications
Drugs like norepinephrine are used to manage persistent hypotension.
4. Source Control
Identify and eliminate the infection source, such as draining abscesses or removing infected devices.
5. Supportive Care
Provide oxygen therapy, mechanical ventilation, or renal replacement therapy as needed.
Prevention of Bacterial Sepsis
Prevention strategies reduce the incidence and severity of bacterial sepsis. Key measures include:
- Vaccination: Immunizations against common pathogens like pneumococcus and meningococcus.
- Infection control: Adhering to hygiene practices, particularly in healthcare settings.
- Chronic disease management: Monitoring and controlling conditions like diabetes or hypertension.
- Prompt treatment of infections: Early intervention for minor infections to prevent escalation.