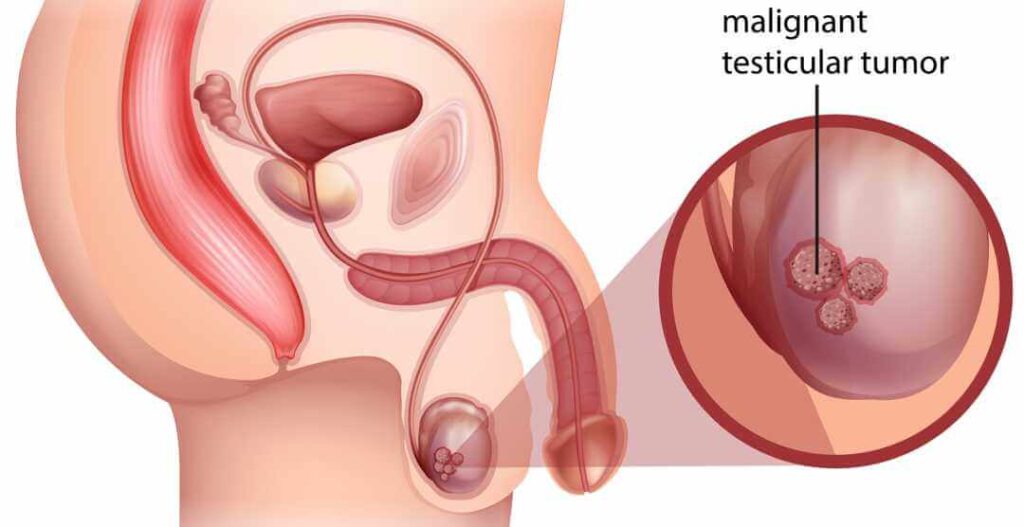
A malignant tumor of the testis, commonly referred to as testicular cancer, is a condition where cancerous cells develop in the testicular tissues. Although rare compared to other malignancies, testicular cancer is the most common cancer among young men aged 15 to 35. Understanding its causes, symptoms, diagnosis, and treatment options is crucial for early detection and effective management.
Types of Malignant Testicular Tumors
Testicular cancer is primarily classified into two main types:
1. Seminomas
- Slow-growing tumors that generally occur in men aged 30–40
- Highly responsive to radiation and chemotherapy
- Usually confined to the testes at diagnosis
2. Non-Seminomas
- More aggressive than seminomas
- Typically affect younger men, aged 15–30
- Includes subtypes such as:
- Embryonal carcinoma
- Yolk sac tumor
- Choriocarcinoma
- Teratoma
Risk Factors and Causes
Several factors can increase the likelihood of developing testicular cancer:
- Cryptorchidism (Undescended Testicle): Men with undescended testes are at a significantly higher risk.
- Family History: A genetic predisposition increases the chances.
- Age: Most cases occur between 15 and 35 years of age.
- Race: Caucasian men have a higher risk than other ethnic groups.
- HIV Infection: Increased risk due to immune system compromise.
Symptoms of Malignant Testicular Tumor
Early detection is crucial. Symptoms include:
- Painless lump or swelling in the testicle
- Heaviness or discomfort in the scrotum
- Pain in the lower abdomen or groin
- Enlargement or tenderness in breast tissue (gynecomastia)
- Sudden fluid accumulation in the scrotum
Diagnostic Procedures
Early diagnosis improves treatment success. Common diagnostic methods include:
- Physical Examination: Checks for lumps, swelling, and asymmetry.
- Ultrasound: Determines if the mass is solid or fluid-filled.
- Blood Tests: Tumor markers like AFP (alpha-fetoprotein), hCG (human chorionic gonadotropin), and LDH (lactate dehydrogenase) help in diagnosis.
- Biopsy: Rarely performed due to the risk of spreading cancer.
- CT Scans/MRI: Detects metastasis in lymph nodes, lungs, and other organs.
Treatment Options
Treatment depends on cancer type and stage:
1. Surgery (Orchiectomy)
- The primary treatment involves removing the affected testicle.
- In advanced cases, retroperitoneal lymph node dissection (RPLND) is performed.
2. Radiation Therapy
- Mainly used for seminomas
- Targets remaining cancer cells after surgery
- Side effects include fatigue, nausea, and infertility
3. Chemotherapy
- Preferred for non-seminomas and advanced seminomas
- Common drugs: Cisplatin, Bleomycin, Etoposide
- Side effects: Hair loss, nausea, neuropathy
4. Surveillance
- Regular check-ups with imaging and blood tests for early relapse detection
- Recommended for low-risk patients post-surgery
Prognosis and Survival Rate
Testicular cancer has one of the highest cure rates among all cancers. The 5-year survival rate is approximately 95%. Early detection further increases this rate to nearly 99% for localized tumors.
Prevention Strategies
Although not all cases are preventable, some measures help lower risk:
- Perform Regular Self-Exams: Early lump detection improves outcomes.
- Address Cryptorchidism in Childhood: Surgery (orchiopexy) reduces testicular cancer risk.
- Avoid Harmful Environmental Exposures: Limit exposure to endocrine disruptors and toxins.
A malignant tumor of the testis is a serious but highly treatable condition, especially when diagnosed early. Regular self-examinations, awareness of risk factors, and prompt medical evaluation for any testicular changes significantly enhance survival rates. If you experience any symptoms, consult a healthcare provider immediately for proper assessment and management.