Malignant neoplasm of the ovary, commonly known as ovarian cancer, is a life-threatening disease that originates in the ovarian tissues. It is the fifth leading cause of cancer-related deaths among women and is often diagnosed at an advanced stage due to its asymptomatic nature in early development.
Causes and Risk Factors
The exact cause of ovarian cancer is unknown, but several risk factors increase susceptibility:
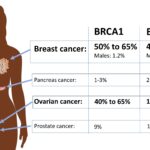
- Genetic Mutations: BRCA1 and BRCA2 gene mutations significantly raise the risk.
- Family History: Women with a history of ovarian, breast, or colorectal cancer in their family are at higher risk.
- Age: The majority of cases occur in women over 50.
- Hormonal Factors: Early menstruation, late menopause, and hormone replacement therapy (HRT) increase risk.
- Obesity: Being overweight may contribute to hormonal imbalances that promote tumor growth.
Symptoms of Ovarian Cancer
Ovarian cancer often presents vague symptoms that mimic other conditions, leading to late diagnosis. Key symptoms include:
- Persistent bloating and abdominal discomfort
- Pelvic pain and pressure
- Loss of appetite or feeling full quickly
- Frequent urination
- Unexplained weight loss
- Fatigue
Types of Malignant Ovarian Tumors
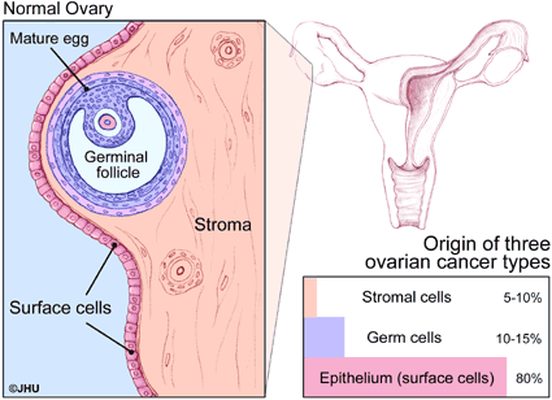
There are several types of ovarian malignancies, classified based on cell origin:
- Epithelial Ovarian Cancer: The most common, originating from the ovarian surface cells.
- Germ Cell Tumors: Arising from egg-producing cells, more common in younger women.
- Stromal Tumors: Developing from hormone-producing cells within the ovary.
Diagnosis and Staging
Diagnosing ovarian cancer requires a combination of imaging, lab tests, and biopsies.
- Pelvic Examination: Initial physical check for abnormalities.
- Ultrasound & CT Scan: Imaging tests to detect tumor size and spread.
- CA-125 Blood Test: A tumor marker elevated in ovarian cancer cases.
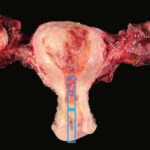
- Biopsy & Histopathology: Definitive diagnosis through tissue examination.
Treatment Options
Treatment plans are personalized based on cancer stage, patient health, and tumor characteristics.
1. Surgery
- Oophorectomy: Removal of one or both ovaries.
- Hysterectomy: Complete removal of the uterus and ovaries in advanced cases.
- Debulking Surgery: Removing as much tumor tissue as possible.
2. Chemotherapy
- Administered before (neoadjuvant) or after (adjuvant) surgery.
- Common drugs include platinum-based agents like carboplatin and cisplatin.
3. Targeted Therapy
- PARP inhibitors (e.g., olaparib) are effective for BRCA-mutated ovarian cancer.
- Bevacizumab (Avastin) inhibits blood vessel growth to tumors.
4. Radiation Therapy
- Used in rare cases for localized tumors or palliative care.
5. Immunotherapy
- Clinical trials are exploring immune checkpoint inhibitors to enhance immune response.
Prognosis and Survival Rates
The prognosis for ovarian cancer depends on the stage at diagnosis:
- Stage I: 90% five-year survival rate.
- Stage II: 70% five-year survival rate.
- Stage III: 39% five-year survival rate.
- Stage IV: Less than 20% five-year survival rate.
Early detection significantly improves outcomes. Regular screening, genetic testing, and lifestyle modifications can aid in prevention.
Malignant neoplasm of the ovary remains a major health concern due to late-stage detection and aggressive nature. Awareness, early diagnosis, and advanced treatments are key to improving survival rates. Women at risk should consult healthcare providers for screening and preventive measures.