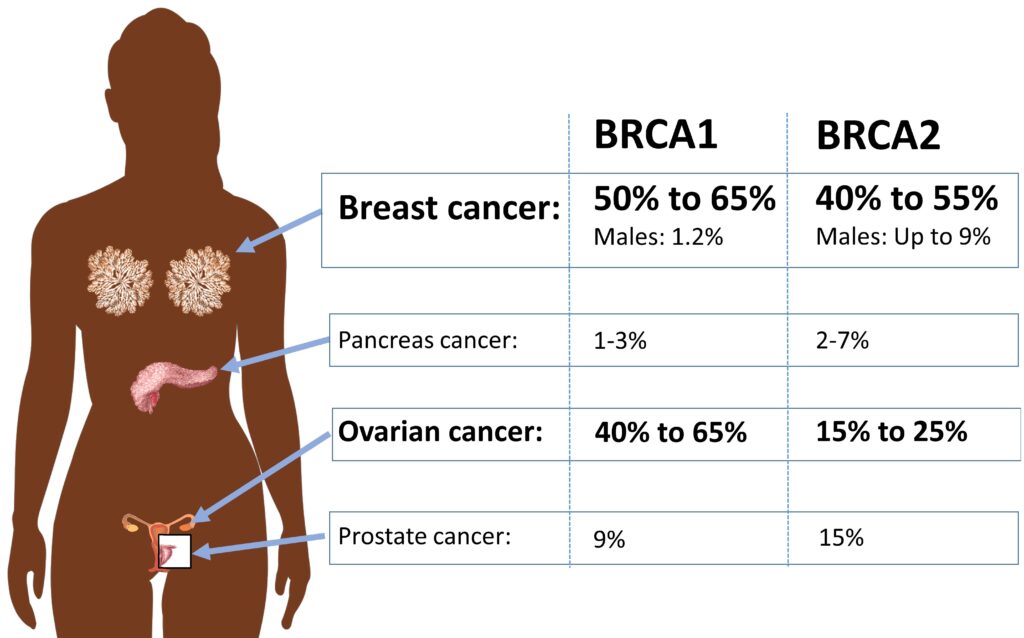
Malignant neoplasms of the ovary are among the most fatal gynecologic malignancies, and mutations in the BRCA1 and BRCA2 genes significantly increase the risk. Women with germline BRCA mutations have a higher likelihood of developing high-grade serous ovarian carcinoma, which represents the most aggressive subtype. Understanding the connection between BRCA mutations and ovarian cancer is crucial for early detection, risk management, and targeted therapy.
BRCA Mutations and Ovarian Cancer Risk
BRCA1 and BRCA2 are tumor suppressor genes responsible for DNA repair. Germline mutations in these genes impair the ability to fix DNA damage, leading to uncontrolled cell growth and cancer development.
- BRCA1 mutation: Increases ovarian cancer risk by 39–44%
- BRCA2 mutation: Increases ovarian cancer risk by 11–17%
These mutations are inherited in an autosomal dominant pattern, meaning a woman with a single mutated copy has a high risk of developing ovarian malignancy.
Symptoms of Ovarian Cancer in BRCA Mutation Carriers
Ovarian cancer often presents with vague symptoms, making early detection challenging. Common symptoms include:
- Abdominal bloating and distension
- Pelvic pain or pressure
- Unexplained weight loss
- Changes in bowel habits
- Frequent urination
- Fatigue
Since these symptoms mimic benign conditions, BRCA mutation carriers should undergo regular screenings for early detection.
Diagnostic Approaches
Early diagnosis improves survival rates. The following diagnostic tools are essential for detecting ovarian neoplasms:
- Transvaginal Ultrasound (TVUS): Detects ovarian masses and abnormal growths.
- CA-125 Blood Test: Elevated levels may indicate ovarian cancer.
- Genetic Testing: Identifies BRCA mutations in at-risk individuals.
- Pelvic MRI or CT Scan: Determines tumor size and spread.
- Biopsy & Histopathology: Confirms malignancy and subtype.
Treatment Strategies for BRCA-Associated Ovarian Cancer
Treatment for ovarian cancer varies based on tumor stage, grade, and BRCA mutation status. Standard approaches include:
1. Surgical Intervention
- Debulking Surgery: Removes as much tumor as possible to enhance therapy efficacy.
- Risk-Reducing Salpingo-Oophorectomy (RRSO): Preventative surgery recommended for high-risk BRCA carriers.
2. Chemotherapy
- Platinum-Based Chemotherapy (Carboplatin + Paclitaxel): First-line treatment.
- Neoadjuvant Therapy: Administered before surgery to shrink tumors.
3. Targeted Therapy with PARP Inhibitors
Poly(ADP-ribose) polymerase (PARP) inhibitors exploit BRCA-mutated cancer cells’ inability to repair DNA damage, leading to cell death.
FDA-Approved PARP Inhibitors:
- Olaparib (Lynparza) – First-line & maintenance therapy
- Rucaparib (Rubraca) – Recurrent BRCA-mutated cases
- Niraparib (Zejula) – Maintenance for all HRD+ tumors
4. Immunotherapy & Clinical Trials
- Checkpoint Inhibitors (PD-1/PD-L1 Blockers): Under research for efficacy in ovarian cancer.
- Experimental Therapies: Combination regimens in clinical trials may improve survival.
Prognosis and Survival Rates
Women with BRCA-associated ovarian cancer often respond better to platinum chemotherapy and PARP inhibitors, resulting in improved progression-free survival (PFS).
| Factor | BRCA1 Mutation | BRCA2 Mutation |
|---|---|---|
| Platinum Sensitivity | High | Very High |
| Median PFS (months) | ~21-25 | ~25-30 |
| Long-Term Survival | Better than sporadic cases | Better than BRCA1 |
Despite better treatment responses, recurrence rates remain high, necessitating continuous follow-up.
Preventive Measures and Risk Management
Women with germline BRCA mutations can take proactive steps to lower their risk:
- RRSO (Removal of ovaries & fallopian tubes) by age 35-45
- Oral Contraceptives: Reduce ovarian cancer risk by up to 50%
- Regular Screening: CA-125, TVUS, and genetic counseling
- Lifestyle Modifications: Maintaining a healthy weight and avoiding smoking
Malignant ovarian neoplasms associated with BRCA mutations pose a significant challenge in oncology. Early detection, advanced targeted therapies, and preventive strategies play a pivotal role in improving outcomes for affected women. Genetic counseling and risk assessment remain essential for high-risk individuals, ensuring informed decision-making and better prognosis.