Lymph node-positive colorectal carcinoma (CRC) occurs when cancer cells spread from the primary tumor in the colon or rectum to nearby lymph nodes. This stage signifies a more advanced disease and influences treatment decisions, prognosis, and recurrence risk. Detecting and managing lymph node involvement is crucial to improving patient survival rates.
Pathophysiology of Lymph Node Metastasis
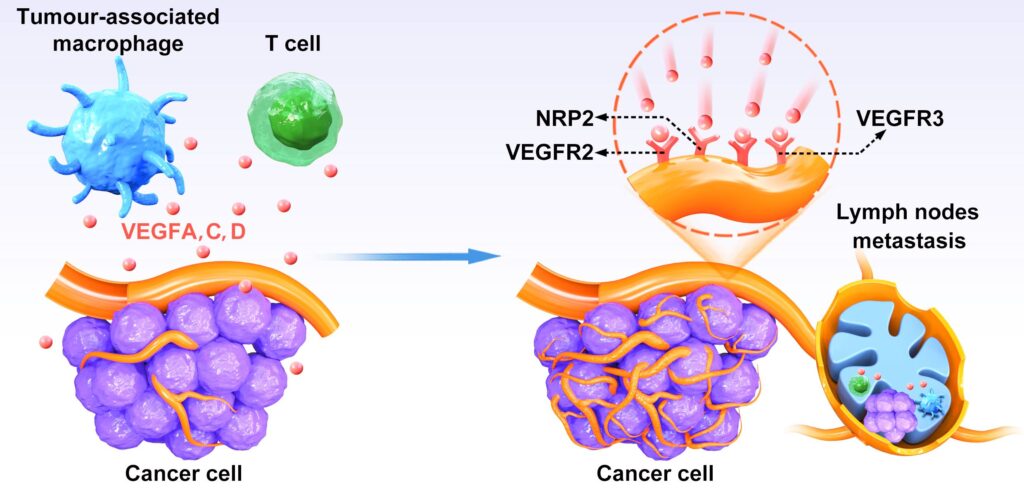
Colorectal cancer typically originates from adenomatous polyps that undergo malignant transformation. As the tumor grows, cancerous cells may infiltrate lymphatic vessels, allowing dissemination to regional lymph nodes. The presence of tumor cells in lymph nodes indicates a higher likelihood of distant metastasis.
Staging of Lymph Node-Positive Colorectal Carcinoma
Lymph node involvement is classified under the TNM (Tumor, Node, Metastasis) staging system:
- N0 – No regional lymph node metastasis
- N1 – Cancer has spread to 1-3 lymph nodes
- N2 – Cancer has spread to 4 or more lymph nodes
Based on these findings, lymph node-positive CRC corresponds to Stage III disease, which is further divided into:
- Stage IIIA – Tumor penetrates the submucosa or muscularis propria with N1 involvement.
- Stage IIIB – Tumor invades through the muscularis propria into adjacent structures with N1 or N2 involvement.
- Stage IIIC – Tumor extends beyond the serosa with extensive lymph node metastasis.
Diagnostic Methods for Lymph Node-Positive CRC
1. Histopathological Examination
Lymph node assessment is performed post-surgical resection. The minimum recommended number of lymph nodes examined is 12 to ensure accurate staging. Hematoxylin and eosin (H&E) staining and immunohistochemistry (IHC) are used to confirm metastases.
2. Imaging Modalities
Non-invasive imaging helps determine lymph node involvement preoperatively:
- Computed Tomography (CT) Scan – Identifies enlarged lymph nodes (>10 mm).
- Magnetic Resonance Imaging (MRI) – Useful for rectal cancer staging.
- Positron Emission Tomography (PET) Scan – Detects metabolically active metastatic lymph nodes.
3. Sentinel Lymph Node Mapping
Emerging techniques such as sentinel lymph node biopsy (SLNB) help assess microscopic metastases in early-stage disease.
Treatment Strategies for Lymph Node-Positive Colorectal Cancer
1. Surgical Resection
Radical colectomy (for colon cancer) and total mesorectal excision (TME) (for rectal cancer) remain the primary treatments. Lymphadenectomy is performed to remove affected nodes and prevent further spread.
2. Adjuvant Chemotherapy
Since Stage III CRC has a high recurrence risk, adjuvant chemotherapy is essential:
- FOLFOX (5-FU, Leucovorin, Oxaliplatin) – Standard first-line therapy.
- CAPOX (Capecitabine, Oxaliplatin) – Alternative regimen.
- FOLFIRI (5-FU, Leucovorin, Irinotecan) – Used in high-risk cases.
Chemotherapy reduces recurrence and increases survival rates, particularly in patients with N2 disease.
3. Radiation Therapy
For rectal cancer, neoadjuvant chemoradiation (chemotherapy + radiation) is recommended before surgery to shrink tumors and reduce lymph node involvement. Postoperative radiation is considered in select cases.
4. Targeted Therapy
Biologic agents are used for advanced cases with specific molecular markers:
- Anti-EGFR Therapy (Cetuximab, Panitumumab) – Used in KRAS wild-type tumors.
- Anti-VEGF Therapy (Bevacizumab) – Inhibits angiogenesis in metastatic disease.
5. Immunotherapy
For patients with microsatellite instability-high (MSI-H) or mismatch repair-deficient (dMMR) tumors, immune checkpoint inhibitors such as pembrolizumab or nivolumab provide effective treatment alternatives.
Prognosis and Survival Rates
The number of affected lymph nodes significantly impacts prognosis:
- N1 (1-3 nodes involved) – 5-year survival: 67-72%
- N2 (≥4 nodes involved) – 5-year survival: 50-58%
Factors influencing survival include:
✔️ Tumor Grade – High-grade tumors have worse outcomes.
✔️ Lymphovascular Invasion (LVI) – Presence worsens prognosis.
✔️ Response to Chemotherapy – Good response improves survival.
Emerging Research and Future Directions
1. Liquid Biopsy for Early Detection
Circulating tumor DNA (ctDNA) is being investigated as a non-invasive biomarker for detecting lymph node metastasis preoperatively.
2. Artificial Intelligence in Staging
AI-based imaging algorithms enhance lymph node assessment accuracy in preoperative scans, improving staging reliability.
3. Personalized Treatment Approaches
Gene expression profiling is helping identify high-risk patients who may benefit from intensified chemotherapy regimens.
Frequently Asked Questions:
1. How is lymph node-positive colorectal carcinoma diagnosed?
Diagnosis is based on surgical pathology, imaging (CT, MRI, PET), and lymph node biopsy.
2. What is the best treatment for Stage III colorectal cancer?
A combination of surgery and adjuvant chemotherapy (FOLFOX or CAPOX) is the standard of care.
3. Can colorectal cancer with lymph node involvement be cured?
Yes, Stage III CRC is curable with aggressive treatment, but recurrence risk remains.
4. What is the role of immunotherapy in lymph node-positive CRC?
It is used in MSI-H/dMMR tumors, which respond well to checkpoint inhibitors like pembrolizumab.
5. How does lymph node involvement affect prognosis?
More lymph node involvement (N2 stage) correlates with a higher risk of recurrence and lower survival rates.