Lyme disease is a bacterial infection caused by Borrelia burgdorferi, transmitted through the bite of infected black-legged ticks (Ixodes scapularis). When the infection spreads to the central nervous system (CNS), it leads to neurological Lyme disease, also known as Lyme neuroborreliosis. This condition affects the brain, spinal cord, and peripheral nerves, potentially causing severe cognitive, motor, and sensory impairments.
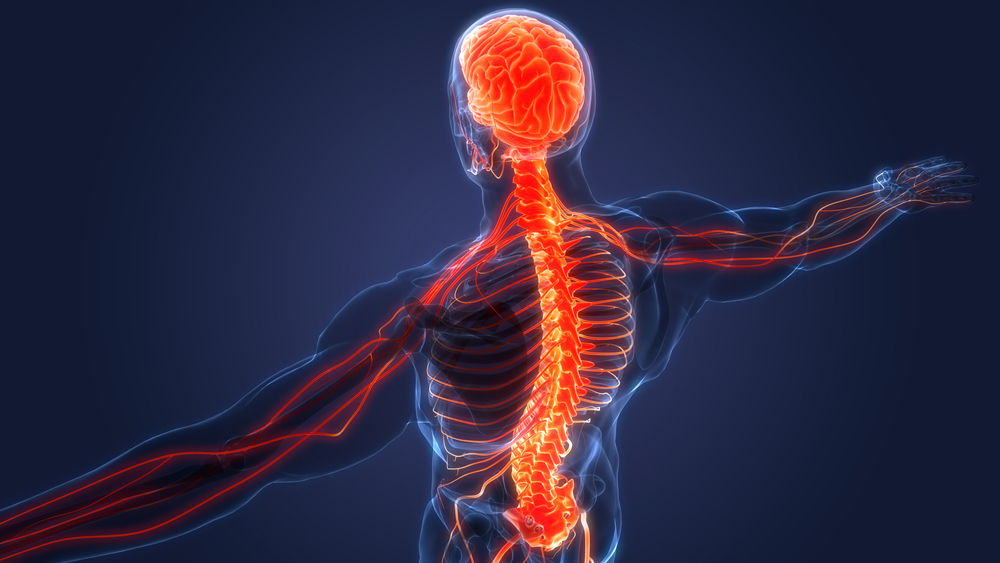
How Lyme Disease Affects the Central Nervous System
Lyme disease can penetrate the CNS through blood circulation, leading to inflammation and neurological dysfunction. The most common manifestations include:
- Meningitis – Inflammation of the membranes surrounding the brain and spinal cord.
- Encephalopathy – Brain dysfunction causing cognitive and memory issues.
- Radiculoneuropathy – Nerve root inflammation leading to pain, weakness, and numbness.
- Cranial Neuritis – Facial paralysis (Bell’s palsy) or vision and hearing problems.
Pathophysiology of CNS Lyme Disease
- Borrelia burgdorferi enters the bloodstream.
- The bacteria cross the blood-brain barrier.
- The immune system triggers an inflammatory response.
- Neurons, myelin, and nerve roots become affected, causing neurological symptoms.
Symptoms of Neurological Lyme Disease
The symptoms vary based on the affected part of the CNS and the stage of the disease.
Early Neurological Symptoms (Weeks to Months After Infection)
- Severe headaches and neck stiffness (Lyme meningitis)
- Facial paralysis (Bell’s palsy) – Drooping on one or both sides of the face
- Radicular pain – Shooting nerve pain in limbs or back
- Cognitive impairment – Difficulty concentrating, brain fog, and confusion
Chronic or Late-Stage Symptoms (Months to Years After Infection)
- Chronic fatigue and weakness
- Memory loss and difficulty processing information
- Seizures and abnormal movements
- Autonomic dysfunction – Irregular heartbeat, dizziness, or low blood pressure
- Psychiatric symptoms – Depression, anxiety, and mood disturbances
Diagnosis of CNS Lyme Disease
Diagnosing Lyme neuroborreliosis is challenging as symptoms overlap with other neurological disorders. Physicians use a combination of clinical evaluation and laboratory tests.
Key Diagnostic Methods
- Serological Tests
- ELISA (Enzyme-Linked Immunosorbent Assay) – Detects Lyme disease antibodies.
- Western Blot Test – Confirms positive ELISA results.
- Lumbar Puncture (Spinal Tap)
- Analyzes cerebrospinal fluid (CSF) for increased white blood cells and Borrelia antibodies.
- Magnetic Resonance Imaging (MRI)
- Identifies brain and spinal cord inflammation or lesions.
- Electromyography (EMG) and Nerve Conduction Studies (NCS)
- Detects nerve damage or dysfunction.
Treatment Options for CNS Lyme Disease
Antibiotic Therapy
- Intravenous (IV) antibiotics – Preferred for severe cases involving the CNS. Common choices include:
- Ceftriaxone – Administered for 2-4 weeks to penetrate the blood-brain barrier.
- Cefotaxime or Penicillin G – Alternatives for IV therapy.
- Oral antibiotics – Doxycycline, amoxicillin, or cefuroxime for milder cases.
Symptomatic and Supportive Treatment
- Corticosteroids – To reduce severe inflammation.
- Pain management – NSAIDs and neuropathic pain medications (gabapentin).
- Physical therapy – Helps regain motor function and prevent muscle atrophy.
- Cognitive rehabilitation – Supports memory and concentration issues.
Prevention Strategies
Since Lyme disease is preventable, reducing tick exposure is critical.
- Use insect repellents – Apply DEET or permethrin to clothing and exposed skin.
- Wear protective clothing – Long-sleeved shirts, pants, and closed-toe shoes.
- Check for ticks regularly – Examine the body, especially behind ears, underarms, and the scalp.
- Remove ticks properly – Use fine-tipped tweezers to extract the tick without squeezing its body.
- Tick-proof your yard – Keep grass short and use tick-control pesticides in high-risk areas.
Complications of Untreated CNS Lyme Disease
Failure to treat Lyme neuroborreliosis can lead to long-term damage, including:
- Chronic neuroinflammation – Persistent brain inflammation causing cognitive dysfunction.
- Peripheral neuropathy – Nerve damage leading to chronic pain and numbness.
- Seizures and epilepsy – Rare cases where Lyme disease triggers neurological seizures.
- Post-Treatment Lyme Disease Syndrome (PTLDS) – Lingering fatigue, joint pain, and cognitive issues despite treatment.
Frequently Asked Questions:
1. Can Lyme disease cause permanent brain damage?
If left untreated, CNS Lyme disease can result in long-term cognitive and neurological impairment, but early treatment reduces the risk.
2. How long does it take for Lyme disease to affect the nervous system?
Neurological symptoms can appear weeks to months after the initial tick bite, depending on the progression of the infection.
3. What is the best treatment for neurological Lyme disease?
IV antibiotics, such as ceftriaxone, are the most effective treatment for severe neurological cases.
4. Can Lyme disease be misdiagnosed as multiple sclerosis (MS)?
Yes, Lyme neuroborreliosis can mimic MS, ALS, and Parkinson’s disease, making differential diagnosis essential.
5. Is chronic neurological Lyme disease real?
Some patients experience persistent symptoms, known as Post-Treatment Lyme Disease Syndrome (PTLDS), even after completing antibiotic therapy.