Biliary tract infections, also referred to as biliary infections or cholangitis, occur when bacteria or other pathogens invade the biliary system. This complex network includes the bile ducts, gallbladder, and associated structures responsible for bile production and transportation. Prompt diagnosis and treatment are crucial to prevent severe complications such as sepsis or liver damage.
Anatomy of the Biliary System
The biliary system comprises the following components:
- Liver: Produces bile, essential for fat digestion.
- Gallbladder: Stores and concentrates bile.
- Bile Ducts: Channels bile from the liver and gallbladder to the small intestine.
This network plays a critical role in digestion and detoxification, making its integrity vital for overall health.
Causes of Biliary Tract Infections
Biliary tract infections typically arise from a combination of factors, including:
- Bile Duct Obstruction: Stones, strictures, or tumors can block bile flow, creating an environment for bacterial growth.
- Bacterial Contamination: Common pathogens include Escherichia coli, Klebsiella pneumoniae, and Enterococcus species.
- Underlying Conditions: Chronic illnesses such as diabetes or cirrhosis may increase susceptibility.
- Medical Procedures: Interventions like endoscopic retrograde cholangiopancreatography (ERCP) can introduce bacteria into the biliary system.
Symptoms and Clinical Presentation
The clinical manifestations of biliary tract infections can vary but often include:
- Fever and Chills: Indicative of systemic infection.
- Jaundice: Yellowing of the skin and eyes due to bile flow obstruction.
- Abdominal Pain: Localized to the right upper quadrant.
- Nausea and Vomiting: Common nonspecific symptoms.
- Dark Urine and Pale Stools: Signs of bile duct obstruction.
Severe cases may progress to septic shock, characterized by low blood pressure and organ dysfunction.
Diagnosis of Biliary Tract Infections
Timely and accurate diagnosis is essential. Key diagnostic steps include:
1. Clinical Evaluation
A thorough patient history and physical examination focusing on characteristic symptoms like fever, jaundice, and abdominal pain.
2. Laboratory Tests
- Blood Tests: Elevated white blood cell count, bilirubin, and liver enzymes.
- Blood Cultures: Identify causative pathogens.
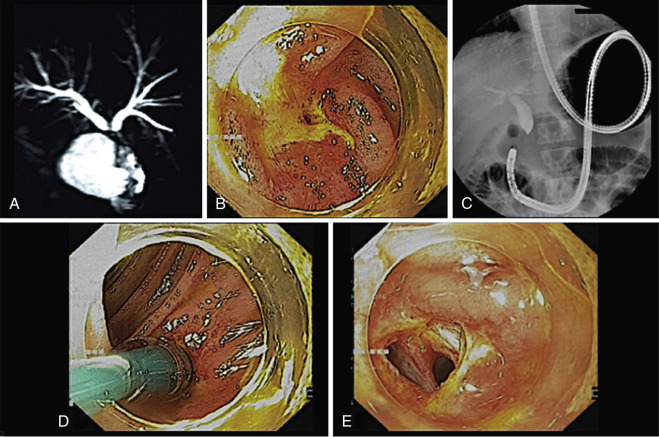
3. Imaging Studies
- Ultrasound: Detects gallstones or bile duct dilation.
- CT Scan: Provides detailed cross-sectional images.
- MRCP: Non-invasive visualization of the biliary system.
Treatment Options
Effective management of biliary tract infections requires a multidisciplinary approach:
1. Antibiotic Therapy
Broad-spectrum antibiotics targeting gram-negative and anaerobic bacteria are the first-line treatment. Common regimens include:
- Piperacillin-tazobactam
- Ceftriaxone with metronidazole
- Carbapenems for severe cases
2. Biliary Drainage
Relieving bile duct obstruction is crucial. Methods include:
- ERCP: Endoscopic removal of stones or placement of stents.
- Percutaneous Drainage: Alternative for inaccessible obstructions.
3. Surgical Intervention
In cases of recurrent infections or structural anomalies, cholecystectomy or reconstructive surgery may be necessary.
Prevention Strategies
Reducing the risk of biliary tract infections involves:
- Timely Management of Gallstones: Prevent bile duct obstruction.
- Hygienic Practices in Medical Procedures: Minimizes infection risks.
- Routine Monitoring: Essential for patients with chronic biliary diseases.
Represent a serious health concern requiring prompt recognition and management. By understanding the anatomy, causes, symptoms, and treatment options, patients and healthcare providers can work together to ensure optimal outcomes. Proactive prevention and timely intervention remain critical pillars of effective care.