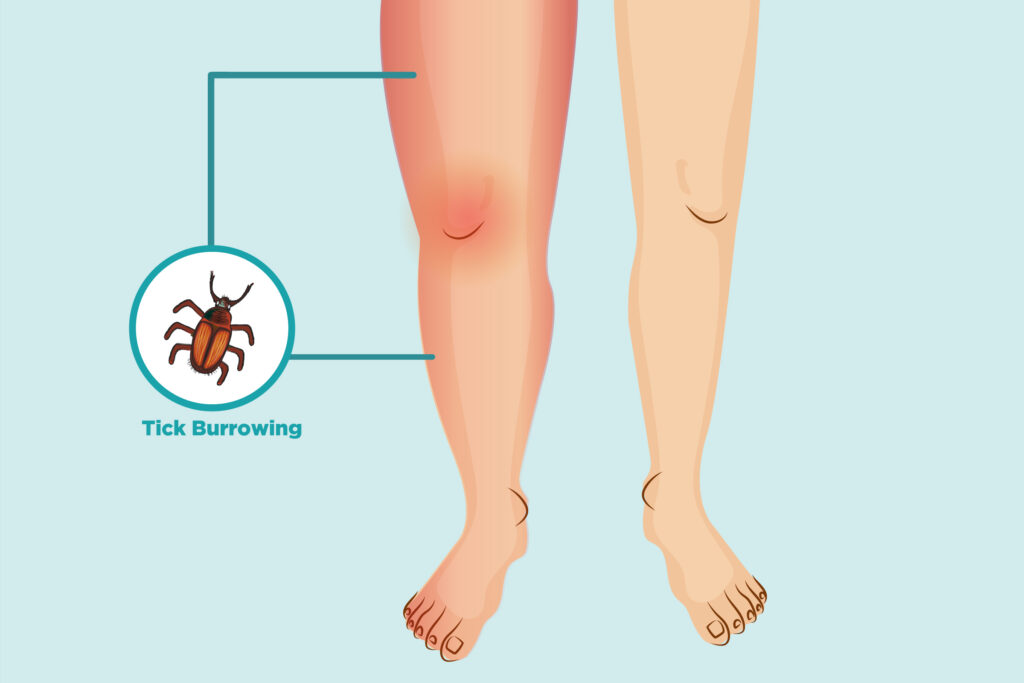
Lyme arthritis is a late-stage complication of Lyme disease, a bacterial infection caused by Borrelia burgdorferi and transmitted through tick bites. It primarily affects the joints, leading to inflammation, swelling, and pain. Early detection and treatment are crucial in preventing long-term complications.
Causes and Pathophysiology
Lyme arthritis occurs when Borrelia burgdorferi bacteria infiltrate the joints, triggering an immune response that results in persistent inflammation. If left untreated, the bacteria can disseminate, leading to chronic joint damage.
Symptoms of Lyme Arthritis
The symptoms of Lyme arthritis develop weeks to months after the initial tick bite. Key indicators include:
- Joint Swelling – Affected joints, particularly the knees, become swollen and tender.
- Intermittent Pain – Episodes of joint pain that come and go.
- Stiffness and Reduced Mobility – Difficulty moving the affected joint due to inflammation.
- Warmth and Redness – Inflamed joints may feel warm and appear red.
- Fatigue and Malaise – Some individuals experience general tiredness and discomfort.
Diagnosis of Lyme Arthritis
Diagnosing Lyme arthritis requires a combination of clinical evaluation and laboratory testing.
Clinical Assessment
- Medical history review, focusing on tick exposure and previous Lyme disease symptoms.
- Physical examination of affected joints.
Laboratory Tests
- ELISA (Enzyme-Linked Immunosorbent Assay): Detects Lyme disease antibodies.
- Western Blot: Confirms ELISA results by identifying specific Borrelia burgdorferi proteins.
- Polymerase Chain Reaction (PCR): Identifies bacterial DNA in synovial fluid from affected joints.
- Synovial Fluid Analysis: Differentiates Lyme arthritis from other inflammatory joint conditions.
Treatment Options
Early intervention is essential to prevent complications. Treatment includes:
Antibiotic Therapy
- Oral Antibiotics:
- Doxycycline (for adults and children over 8)
- Amoxicillin (for younger children and pregnant women)
- Cefuroxime axetil (alternative for those allergic to doxycycline)
- Intravenous (IV) Antibiotics:
- Recommended for severe cases unresponsive to oral antibiotics.
- Ceftriaxone or cefotaxime for 2-4 weeks.
Symptomatic Treatment
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Reduce pain and swelling.
- Corticosteroid Injections: Used cautiously in persistent cases.
- Physical Therapy: Helps maintain joint mobility and strength.
Prognosis and Complications
With appropriate antibiotic therapy, most individuals recover fully. However, some patients develop post-treatment Lyme disease syndrome (PTLDS), characterized by persistent joint pain and fatigue despite bacterial eradication.
Complications may include:
- Chronic arthritis if untreated.
- Neurological involvement leading to Lyme neuroborreliosis.
- Autoimmune reactions mimicking rheumatoid arthritis.
Prevention Strategies
Preventing Lyme arthritis begins with avoiding tick bites:
- Wear long clothing in wooded areas.
- Use insect repellents containing DEET or permethrin.
- Perform tick checks after outdoor activities.
- Remove ticks promptly using fine-tipped tweezers.
Lyme arthritis is a serious but treatable manifestation of Lyme disease. Early recognition, prompt antibiotic treatment, and preventive measures are key to reducing its impact. If joint symptoms persist after treatment, consultation with a specialist is recommended to rule out other conditions and manage lingering effects.