Liposarcoma is a rare and malignant tumor originating from fat cells, typically developing in the deep soft tissues of the extremities and the retroperitoneum. It is a subtype of soft tissue sarcoma, accounting for approximately 15% to 20% of all cases within this category. Early detection and comprehensive understanding of liposarcoma are crucial for effective treatment and improved patient outcomes.

Types of Liposarcoma
Liposarcoma is classified into several histological subtypes, each exhibiting distinct clinical behaviors and prognostic implications:
- Well-Differentiated Liposarcoma (WDLPS)/Atypical Lipomatous Tumor (ALT): This is the most prevalent form, characterized by slow growth and a low propensity for metastasis. However, it has a tendency to recur locally after surgical removal.
- Dedifferentiated Liposarcoma (DDLPS): Arising from WDLPS, this subtype exhibits more aggressive behavior with a higher likelihood of metastasis.
- Myxoid Liposarcoma (MLPS): Representing the second most common subtype, MLPS typically grows slowly but can progress to a more aggressive form known as round cell liposarcoma.
- Pleomorphic Liposarcoma (PLPS): This rare and highly aggressive variant accounts for fewer than 5% of liposarcoma cases and is more common in older adults.
- Myxoid Pleomorphic Liposarcoma (MPLPS): A rare combination of myxoid and pleomorphic features, exhibiting variable behavior.
Causes and Risk Factors
The exact etiology of liposarcoma remains unclear. Unlike some other soft tissue sarcomas, radiation exposure does not appear to be a significant risk factor. Genetic abnormalities play a crucial role in the development of liposarcoma, with different subtypes exhibiting distinct chromosomal alterations:
- WDLPS and DDLPS: Characterized by amplifications within chromosome 12, leading to overexpression of oncogenic genes.
- MLPS: Defined by a specific translocation between chromosomes 12 and 16, resulting in the formation of the FUS-DDIT3 fusion protein.
- PLPS: Exhibits complex karyotypic abnormalities with various mutations.
Liposarcoma typically arises de novo rather than from pre-existing benign lipomas.
Symptoms and Clinical Presentation
The clinical manifestations of liposarcoma vary depending on the tumor’s location:
- Extremities (Arms and Legs): Patients may notice a painless, enlarging mass beneath the skin. As the tumor grows, it can cause pain, swelling, and weakness in the affected limb due to compression of adjacent structures.
- Abdomen (Retroperitoneal Space): Tumors in this area may lead to abdominal pain, swelling, early satiety, constipation, and, in some cases, blood in the stool.
Given the potential for liposarcoma to grow significantly before causing noticeable symptoms, any persistent or enlarging mass warrants prompt medical evaluation.
Diagnosis
Accurate diagnosis of liposarcoma involves a combination of imaging studies and histopathological examination:
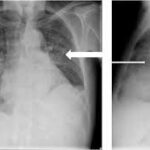
- Imaging Tests: Modalities such as X-rays, computed tomography (CT) scans, and magnetic resonance imaging (MRI) are employed to assess the tumor’s size, location, and involvement of surrounding tissues.
- Biopsy: Definitive diagnosis requires a biopsy, wherein a tissue sample is extracted and analyzed microscopically to determine the tumor’s histological subtype.
Staging studies, including chest imaging, are essential to evaluate for metastatic disease and to guide treatment planning.
Treatment Options
The management of liposarcoma is tailored to the tumor’s subtype, location, and stage. Treatment strategies may include:
- Surgical Resection: The primary treatment for localized liposarcoma involves complete surgical removal of the tumor with clear margins to minimize the risk of recurrence.
- Radiation Therapy: Often employed as an adjunct to surgery, radiation therapy utilizes high-energy beams to destroy residual cancer cells, particularly in cases where achieving clear surgical margins is challenging.
- Chemotherapy: The role of chemotherapy varies among liposarcoma subtypes. While some variants, such as the round cell component of MLPS, may respond to chemotherapeutic agents, others demonstrate limited sensitivity. Chemotherapy may be considered for metastatic or unresectable disease.
- Targeted Therapies and Clinical Trials: Ongoing research into the molecular pathways involved in liposarcoma has led to the development of targeted therapies. Participation in clinical trials may provide access to novel treatments and should be discussed with the oncology care team.
Prognosis and Follow-Up
Prognostic outcomes in liposarcoma are influenced by factors such as tumor subtype, size, location, and the presence of metastatic disease:
- WDLPS/ALT: Generally associated with a favorable prognosis due to its low-grade nature.
- MLPS: Exhibits an intermediate prognosis, with outcomes varying based on the proportion of round cell components.
- PLPS: Carries a poorer prognosis due to its aggressive behavior and higher metastatic potential.
Regular follow-up is imperative, as liposarcoma has a propensity for local recurrence and, in some cases, distant metastasis. Surveillance typically involves periodic imaging and clinical assessments to detect recurrences early and to initiate prompt intervention.
Liposarcoma represents a complex and heterogeneous group of malignant tumors arising from adipose tissue. A comprehensive understanding of its subtypes, clinical presentations, and treatment modalities is essential for optimizing patient care. Multidisciplinary collaboration among surgical oncologists, medical oncologists, radiation oncologists, and pathologists is paramount in devising individualized treatment plans and improving patient outcomes.