Bladder hyperactivity, often referred to as overactive bladder (OAB), is a common condition that significantly impacts the quality of life for millions worldwide. Characterized by frequent and urgent urination, with or without urinary incontinence, OAB can lead to social embarrassment, disrupted daily activities, and psychological distress. This article delves deeply into the condition’s causes, symptoms, diagnosis, and treatment options, offering a comprehensive resource for those seeking clarity and effective management strategies.
What is Bladder Hyperactivity?
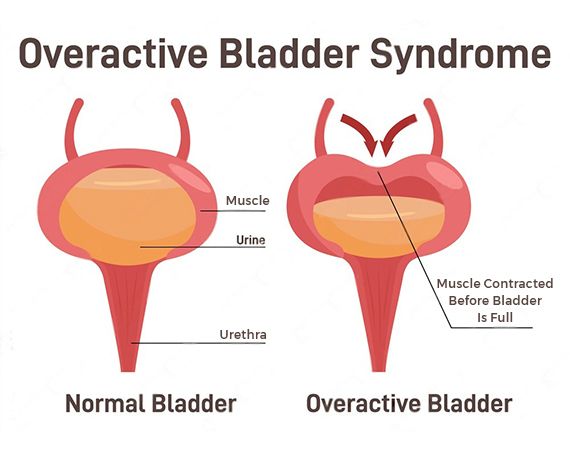
Its a condition where the bladder’s detrusor muscle contracts involuntarily, even when the bladder is not full. This results in a strong, sudden urge to urinate, which can sometimes be difficult to control. Although OAB is not life-threatening, its impact on daily life can be profound, often causing individuals to avoid social settings or experience anxiety about finding restrooms.
Key Symptoms of Bladder Hyperactivity
Individuals with bladder hyperactivity may experience:
- Urinary urgency: A sudden, uncontrollable need to urinate.
- Frequent urination: Needing to urinate more than eight times in 24 hours.
- Nocturia: Waking up multiple times during the night to urinate.
- Urge incontinence: Involuntary loss of urine following a strong urge to urinate.
While these symptoms are common indicators, the severity and combination of symptoms vary among individuals.
Causes of Bladder Hyperactivity
Bladder hyperactivity can arise from various underlying factors, including:
- Neurological conditions: Diseases like Parkinson’s, multiple sclerosis, or stroke can disrupt nerve signals controlling the bladder.
- Aging: The bladder muscle’s elasticity decreases with age, leading to more frequent contractions.
- Bladder outlet obstruction: Conditions such as benign prostatic hyperplasia (BPH) in men can impede normal bladder emptying.
- Hormonal changes: Postmenopausal women often experience changes in bladder function due to decreased estrogen levels.
- Infections: Urinary tract infections (UTIs) can temporarily cause overactive bladder symptoms.
Diagnosis of Bladder Hyperactivity
Accurate diagnosis is essential for effective management. Diagnostic steps include:
- Medical history review: Identifying symptoms, lifestyle habits, and underlying health conditions.
- Physical examination: Assessing pelvic or abdominal health.
- Urinalysis: Detecting infections, blood, or abnormalities in urine.
- Bladder diary: Recording urination patterns and fluid intake.
- Urodynamic testing: Measuring bladder pressure and urine flow to assess functionality.
Treatment Options for Bladder Hyperactivity
Treatment for bladder hyperactivity focuses on alleviating symptoms and improving quality of life. Options include:
Lifestyle Modifications
- Dietary changes: Avoiding caffeine, alcohol, and spicy foods that may irritate the bladder.
- Fluid management: Monitoring and moderating fluid intake.
- Bladder training: Delaying urination to increase bladder capacity.
Pelvic Floor Exercises
Strengthening the pelvic floor muscles through Kegel exercises can help control urination and reduce symptoms.
Medications
- Anticholinergics: Reduce bladder muscle spasms.
- Beta-3 agonists: Relax the bladder muscle to increase storage capacity.
- Topical estrogen: For postmenopausal women, this can improve bladder health.
Advanced Therapies
- Botox injections: Temporarily paralyze bladder muscles to prevent overactivity.
- Nerve stimulation: Techniques like sacral neuromodulation can regulate bladder nerve signals.
Surgical Interventions
In severe cases, surgical options such as bladder augmentation may be considered to increase bladder capacity.
Preventive Measures
While not all cases of bladder hyperactivity are preventable, adopting healthy habits can reduce risk:
- Maintaining a healthy weight to reduce pressure on the bladder.
- Staying physically active to improve overall bladder function.
- Avoiding bladder irritants, such as tobacco and excessive caffeine.
- Regularly emptying the bladder to prevent overdistension.
Living with Bladder Hyperactivity
Its can be challenging, but it is manageable with proper care and treatment. Building a supportive care team, including healthcare providers and support groups, can make a significant difference in improving the quality of life.