Invasive pulmonary aspergillosis (IPA) is a severe fungal infection caused by Aspergillus species, predominantly affecting immunocompromised individuals. It occurs when fungal spores, inhaled into the lungs, invade lung tissue and spread to other organs. If untreated, IPA has a high mortality rate, making early diagnosis and aggressive antifungal treatment crucial.
Causes and Risk Factors
IPA is caused by Aspergillus fumigatus, a ubiquitous mold found in soil, decaying vegetation, and indoor environments. While healthy individuals can clear Aspergillus spores without complications, immunosuppressed patients face a high risk of invasive infection.
Major Risk Factors:
- Prolonged Neutropenia: Common in chemotherapy patients, leading to impaired immune response.
- Hematologic Malignancies: Leukemia, lymphoma, and multiple myeloma increase susceptibility.
- Stem Cell and Organ Transplantation: Immunosuppressive therapy raises infection risk.
- Corticosteroid Therapy: Prolonged steroid use weakens host defenses.
- Chronic Granulomatous Disease: A genetic immune disorder affecting neutrophil function.
- Severe COVID-19 and Influenza: Viral infections disrupt lung defenses, increasing fungal colonization.
Symptoms of Invasive Pulmonary Aspergillosis
IPA presents with nonspecific respiratory and systemic symptoms, often mimicking bacterial pneumonia or viral infections.
- Persistent Fever: Unresponsive to broad-spectrum antibiotics.
- Cough with Hemoptysis: Blood-tinged sputum due to lung tissue invasion.
- Pleuritic Chest Pain: Sharp pain worsening with breathing or coughing.
- Shortness of Breath: Progressing to respiratory failure in severe cases.
- Fatigue and Weight Loss: Indicative of systemic fungal spread.
In advanced cases, IPA can disseminate to the brain, liver, kidneys, and skin, leading to neurological deficits, organ failure, and life-threatening complications.
Pathogenesis of Invasive Pulmonary Aspergillosis
Upon inhalation, Aspergillus spores bypass immune defenses in immunocompromised hosts, germinate into hyphae, and invade blood vessels, causing tissue necrosis and infarction.
Diagnostic Approach
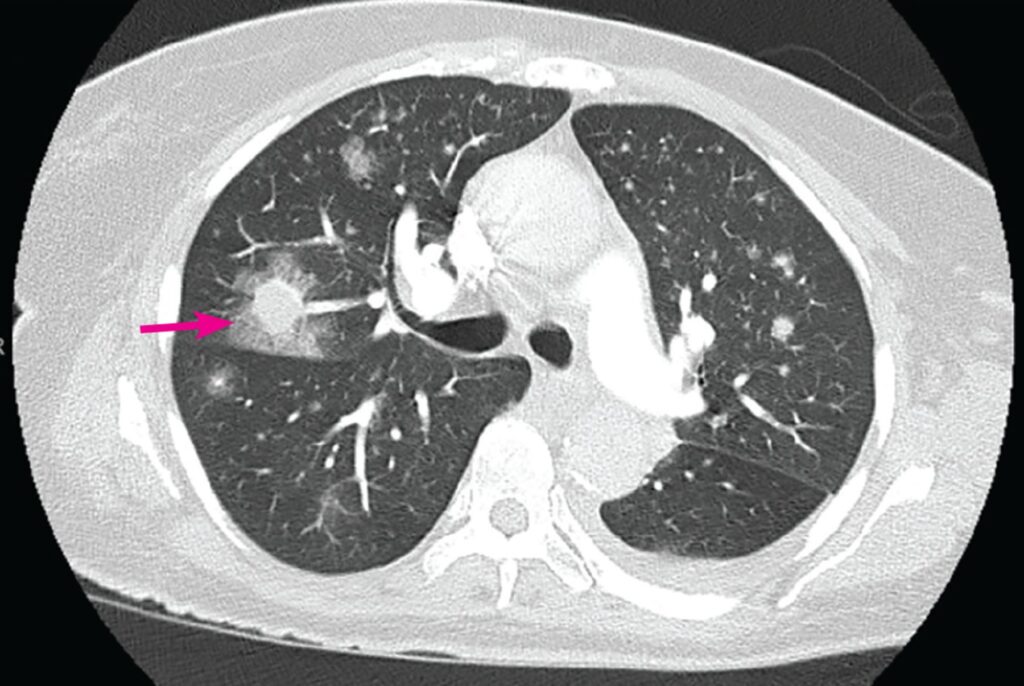
1. Imaging Studies
- Chest CT Scan:
- Early “halo sign” (ground-glass opacity around a nodule)
- Late “air crescent sign” (cavitation within necrotic lung tissue)
- X-ray Findings: Less sensitive but may show nodular or infiltrative patterns.
2. Microbiological and Serological Tests
- Galactomannan Assay: Detects fungal cell wall antigen in serum or bronchoalveolar lavage (BAL).
- Beta-D-Glucan Test: Non-specific but supportive for fungal infections.
- Sputum Culture and PCR: Confirms Aspergillus species, though culture sensitivity is low.
- Bronchoscopy with BAL: Essential for definitive diagnosis in high-risk patients.
3. Histopathology
- Lung Biopsy: Demonstrates septate hyphae with acute-angle branching, confirming invasive disease.
Treatment Strategies for Invasive Pulmonary Aspergillosis
1. Antifungal Therapy
- First-Line Treatment:
- Voriconazole (IV or Oral): Preferred antifungal with superior efficacy.
- Alternative Agents:
- Liposomal Amphotericin B: Used for voriconazole-resistant cases.
- Isavuconazole: Broad-spectrum azole with fewer side effects.
- Combination Therapy:
- Voriconazole + Echinocandin (Caspofungin) in refractory IPA cases.
2. Surgical Intervention
- Indicated in localized necrosis, massive hemoptysis, or resistant lesions.
- Lobectomy may be required for persistent fungal abscesses.
3. Immune System Support
- G-CSF (Granulocyte Colony-Stimulating Factor): Boosts neutrophil recovery.
- Reduction of Immunosuppressive Therapy: When feasible, taper steroids or immunosuppressants.
Prognosis and Survival Rates
Early diagnosis and prompt antifungal therapy significantly impact survival rates:
- Patients with hematologic malignancies: 30–50% mortality
- Hematopoietic stem cell transplant recipients: 50–70% mortality
- Solid organ transplant recipients: 20–40% mortality
- Late-stage or untreated cases: Up to 90% mortality
Improved outcomes depend on:
- Early initiation of voriconazole
- Reversal of immunosuppression
- Aggressive supportive care
Prevention Strategies
- Environmental Control:
- HEPA filtration in hospital settings to minimize fungal exposure.
- Avoidance of construction sites where spores are abundant.
- Antifungal Prophylaxis:
- Voriconazole or posaconazole for high-risk transplant and leukemia patients.
- Monitoring High-Risk Patients:
- Routine galactomannan testing in neutropenic or post-transplant patients.
Invasive pulmonary aspergillosis is a life-threatening fungal infection requiring rapid diagnosis and aggressive antifungal treatment. With advancements in antifungal therapy and early detection, survival rates continue to improve. High-risk patients should receive prophylactic antifungal strategies and close monitoring to prevent fatal complications.