Inclusion conjunctivitis is an ocular infection primarily caused by the bacterium Chlamydia trachomatis. This condition is commonly transmitted through genital-ocular contact but can also result from autoinoculation in individuals with active genital chlamydial infections. Newborns may contract the infection during vaginal delivery from an infected mother.
Causes and Transmission
Inclusion conjunctivitis is caused by specific serovars of Chlamydia trachomatis, particularly D-K types. The infection is transmitted through:
- Genital-ocular contact
- Autoinoculation from infected genital secretions
- Neonatal exposure during childbirth
- Sharing contaminated towels, linens, or cosmetics
Symptoms of Inclusion Conjunctivitis
Symptoms typically appear 5 to 12 days post-exposure and may include:
- Redness and irritation in the affected eye
- Mucopurulent discharge
- Swollen eyelids
- Enlarged preauricular lymph nodes
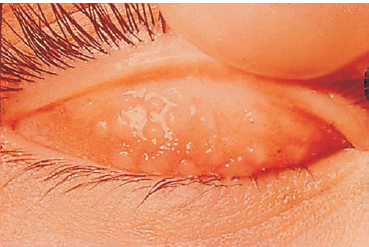
- Follicular conjunctivitis on the inner surface of the eyelid
Risk Factors
The following factors increase the risk of developing inclusion conjunctivitis:
- Unprotected sexual activity
- Concurrent genital chlamydial infection
- Poor hygiene practices
- Exposure to infected individuals
Diagnosis
A comprehensive diagnosis involves:
- Patient History: Identifying sexual history, genital symptoms, or neonatal exposure.
- Physical Examination: Observing ocular discharge, follicular conjunctivitis, and eyelid swelling.
- Laboratory Tests:
- Nucleic acid amplification test (NAAT)
- Polymerase chain reaction (PCR)
- Direct fluorescent antibody (DFA) testing
- Giemsa staining to detect inclusions in conjunctival epithelial cells
Treatment Options
Treatment typically involves:
- Antibiotics: Oral azithromycin or doxycycline for adults. For neonates, erythromycin is preferred.
- Topical Therapy: While systemic treatment is essential, adjunctive topical antibiotics may provide symptomatic relief.
- Partner Notification and Treatment: Essential to prevent reinfection.
Prevention Strategies
Preventive measures include:
- Practicing safe sex
- Screening and treating genital chlamydial infections
- Administering prophylactic erythromycin ointment to newborns born to infected mothers
Complications
Untreated inclusion conjunctivitis can lead to:
- Chronic keratoconjunctivitis
- Corneal scarring
- Visual impairment
- Recurrent conjunctivitis episodes
Epidemiology
Inclusion conjunctivitis is prevalent in sexually active adults and newborns. The condition is often seen in regions with limited access to healthcare or poor sanitation practices.
Inclusion conjunctivitis caused by Chlamydia trachomatis is a treatable yet potentially serious condition requiring timely diagnosis and appropriate management. Early intervention minimizes complications and prevents the spread of infection. Practicing safe sexual behaviors and ensuring effective newborn prophylaxis are key preventive strategies.
FAQs
Q1: How long does inclusion conjunctivitis last?
With appropriate antibiotic treatment, symptoms typically resolve within 1 to 2 weeks.
Q2: Can inclusion conjunctivitis recur?
Yes, reinfection can occur if sexual partners are not treated or hygiene practices are inadequate.
Q3: Is inclusion conjunctivitis contagious?
Yes, the infection can spread through direct contact with infected secretions.
Q4: Can contact lenses worsen inclusion conjunctivitis?
Yes, contact lenses can exacerbate symptoms and delay recovery if worn during an active infection.
Q5: Is inclusion conjunctivitis common in children?
It is more common in newborns due to exposure during childbirth.