Inactive tuberculosis, also known as latent TB infection (LTBI), occurs when an individual is infected with Mycobacterium tuberculosis bacteria but does not exhibit active symptoms. While inactive TB does not cause immediate illness, the bacteria remain dormant in the body and can potentially activate under certain conditions.
Causes and Transmission of Inactive Tuberculosis
Inactive TB develops when an individual is exposed to TB bacteria but their immune system successfully contains the infection. The bacteria remain in a dormant state without causing active disease. Although inactive TB is not contagious, untreated cases may progress to active tuberculosis if the immune system weakens.
Symptoms of Inactive Tuberculosis
Individuals with inactive TB typically exhibit no symptoms. However, in some cases, they may experience:
- Mild fatigue
- Slight chest discomfort
- Occasional cough (rare)
Risk Factors for Developing Active TB
Certain conditions can increase the risk of inactive TB progressing to active TB, including:
- HIV infection or other immune-suppressing conditions
- Diabetes
- Chronic kidney disease
- Malnutrition
- Smoking or substance abuse
- Age-related immune decline
Diagnosis of Inactive Tuberculosis
Diagnosing inactive TB involves specialized tests since patients show no apparent symptoms. Common diagnostic methods include:
- Tuberculin Skin Test (TST): A small injection under the skin, with swelling at the injection site indicating exposure to TB bacteria.
- Interferon-Gamma Release Assays (IGRAs): Blood tests that measure immune response to TB bacteria.
- Chest X-rays or CT Scans: Used to identify lung abnormalities linked to inactive TB.
Treatment Options for Inactive Tuberculosis
Early treatment of inactive TB is crucial in preventing active TB. Treatment options may include:
- Isoniazid (INH): A 6-9 month regimen recommended for most individuals with LTBI.
- Rifampin: A 4-month course suitable for those intolerant to INH.
- Combination Therapy: Rifapentine and INH for a 3-month weekly treatment regimen.
Preventive Measures to Avoid TB Progression
Individuals diagnosed with inactive TB can reduce the risk of developing active TB by following these strategies:
- Completing the prescribed treatment regimen
- Maintaining a healthy immune system through proper nutrition and exercise
- Avoiding exposure to individuals with active TB
- Regular medical check-ups for TB monitoring
Potential Complications of Untreated Inactive Tuberculosis
If inactive TB remains untreated, it may progress to active TB, potentially resulting in severe complications such as:
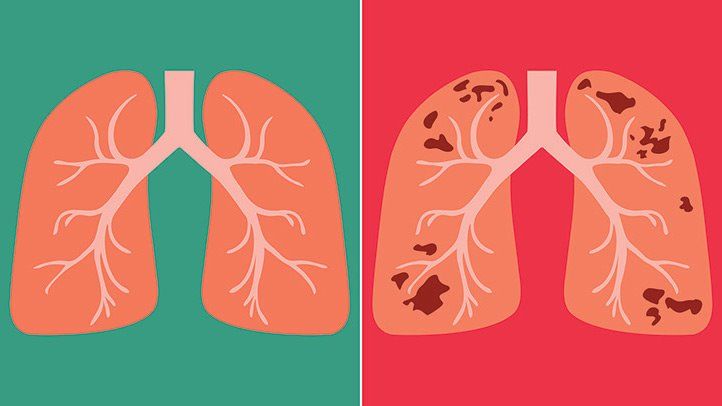
- Lung damage
- Respiratory failure
- Spread of TB bacteria to other organs
Frequently Asked Questions
1. Can inactive TB become active without symptoms?
Inactive TB generally shows no symptoms, but if the immune system weakens, active TB may develop, often beginning with mild symptoms.
2. How long does inactive TB treatment last?
Treatment typically lasts between 3 to 9 months, depending on the prescribed medication regimen.
3. Is inactive TB contagious?
No, inactive TB is not contagious; only active TB can spread to others.
4. Can inactive TB be detected through routine blood tests?
Standard blood tests cannot detect inactive TB; specialized tests like IGRAs are required.
5. Should family members of an individual with inactive TB be tested?
Yes, individuals who have been in close contact with someone diagnosed with inactive TB should undergo testing to assess exposure risk.
Inactive tuberculosis, though non-contagious, poses a potential risk if untreated. Early detection, proper treatment, and lifestyle adjustments are key to preventing its progression to active TB. Seeking medical guidance is essential for effective management and long-term health.