Hypoprothrombinemia is a rare blood disorder characterized by a deficiency in prothrombin (Factor II), a protein essential for blood clotting. This condition can lead to excessive bleeding, bruising, and other complications. Hypoprothrombinemia may be congenital or acquired, and proper diagnosis and treatment are crucial for managing this condition effectively.
Causes of Hypoprothrombinemia
Congenital Causes
- Hereditary Disorders: Congenital hypoprothrombinemia is typically inherited in an autosomal recessive pattern. Mutations in the F2 gene, responsible for prothrombin production, are the primary cause.
- Combined Factor Deficiencies: Conditions like Combined Deficiency of Vitamin K-dependent Factors (VKCFD) can also result in low prothrombin levels.
Acquired Causes
- Vitamin K Deficiency: Vitamin K is essential for synthesizing prothrombin. Deficiencies may occur due to malnutrition, malabsorption disorders, or the use of certain medications (e.g., antibiotics, anticoagulants).
- Liver Disease: Since prothrombin is synthesized in the liver, conditions like cirrhosis or hepatitis can impair its production.
- Anticoagulant Therapy: Drugs such as warfarin reduce prothrombin levels to prevent blood clotting, which can sometimes lead to hypoprothrombinemia.
- Autoimmune Disorders: Conditions that lead to the production of antibodies against clotting factors may also cause this condition.
Symptoms of Hypoprothrombinemia
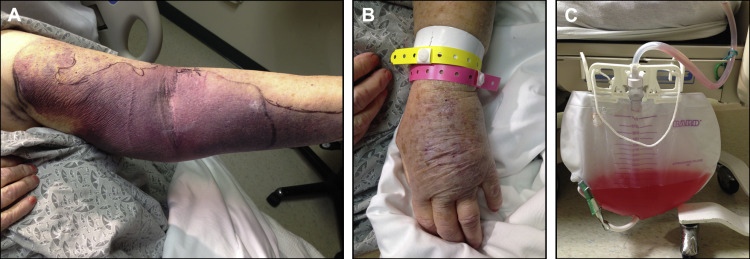
- Prolonged bleeding from cuts or injuries
- Easy bruising without apparent cause
- Nosebleeds or bleeding gums
- Heavy menstrual bleeding in women
- Gastrointestinal bleeding leading to black or bloody stools
- Hematuria (blood in urine)
In severe cases, internal bleeding may occur, posing life-threatening risks.
Diagnosis of Hypoprothrombinemia
Diagnosing hypoprothrombinemia requires a series of blood tests to evaluate clotting function:
- Prothrombin Time (PT): Measures how quickly blood clots; prolonged PT indicates clotting issues.
- Activated Partial Thromboplastin Time (aPTT): Identifies abnormalities in the intrinsic and common coagulation pathways.
- Factor II Assay: Directly measures prothrombin levels to confirm the diagnosis.
Treatment for Hypoprothrombinemia
Vitamin K Therapy
- Administered orally, subcutaneously, or intravenously to correct deficiencies caused by poor diet, malabsorption, or medication use.
Fresh Frozen Plasma (FFP)
- Used in urgent situations where immediate clotting factor replacement is required.
Prothrombin Complex Concentrates (PCC)
- Contain concentrated clotting factors, including Factor II, and are used for severe bleeding episodes.
Managing Underlying Conditions
- For liver disease or autoimmune causes, addressing the root problem is essential for recovery.
Preventing Hypoprothrombinemia
- Balanced Diet: Ensuring adequate intake of Vitamin K through leafy greens, broccoli, and vegetable oils.
- Monitoring Medication Use: Patients on anticoagulants should undergo regular blood tests to manage prothrombin levels safely.
- Managing Chronic Conditions: Treating liver disease or autoimmune disorders promptly can prevent secondary hypoprothrombinemia.
Complications of Hypoprothrombinemia
If untreated, hypoprothrombinemia can lead to severe complications, including:
- Hemorrhagic strokes
- Internal organ bleeding
- Shock due to severe blood loss
- Increased risk of surgical complications
Hypoprothrombinemia and Pregnancy
Pregnant women with hypoprothrombinemia are at greater risk of excessive bleeding during delivery. Careful monitoring, vitamin K supplementation, and proactive obstetric care are crucial for ensuring maternal and fetal health.
Prognosis and Outlook
The prognosis for hypoprothrombinemia largely depends on the underlying cause. With appropriate treatment, patients can manage symptoms effectively. Early diagnosis and consistent medical care improve long-term outcomes.
Hypoprothrombinemia is a serious but manageable condition with timely diagnosis and proper treatment. Understanding its causes, symptoms, and treatment options is crucial for improving patient outcomes and preventing complications.