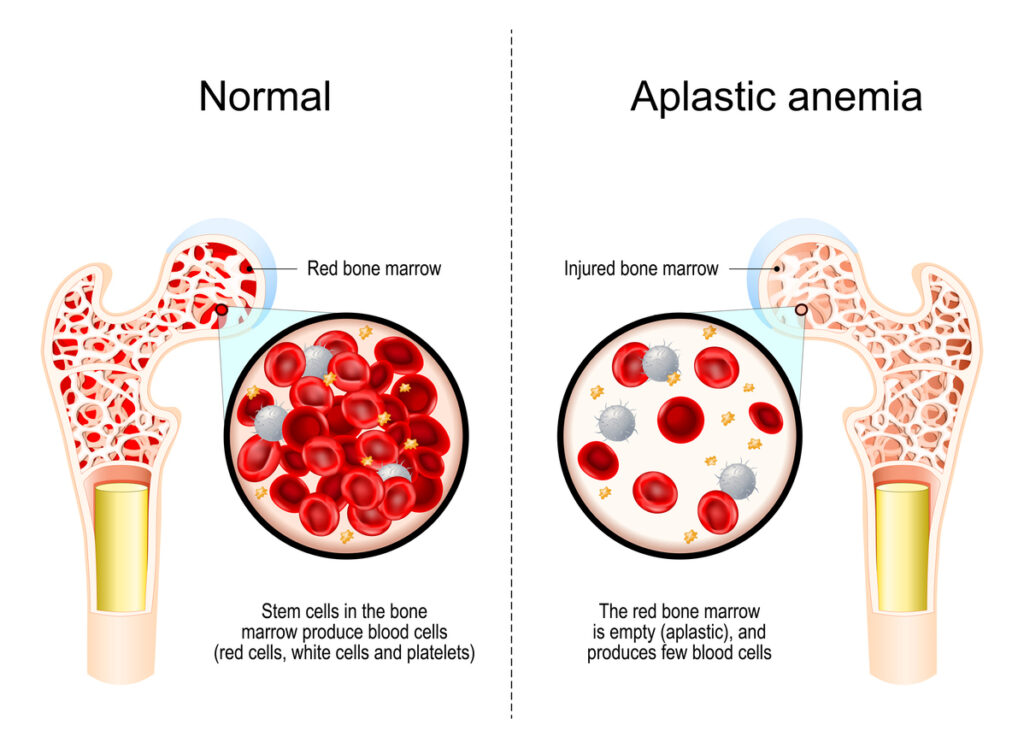
Hypoplastic anemia is a rare blood disorder characterized by reduced bone marrow activity, resulting in decreased production of red blood cells. This condition can lead to severe fatigue, weakness, and compromised immune function.
Causes of Hypoplastic Anemia
The underlying causes of hypoplastic anemia may vary, and they can be categorized as follows:
1. Congenital Causes
- Fanconi anemia – A genetic disorder that affects bone marrow.
- Shwachman-Diamond syndrome – A rare inherited condition that impairs bone marrow function.
2. Acquired Causes
- Chemical exposure – Prolonged contact with benzene, pesticides, or industrial chemicals.
- Medications – Certain antibiotics, chemotherapy drugs, or anticonvulsants.
- Viral Infections – Hepatitis, HIV, Epstein-Barr virus, and Parvovirus B19.
- Radiation exposure – High radiation levels can damage bone marrow cells.
- Autoimmune conditions – Diseases such as lupus may attack bone marrow cells.
Symptoms of Hypoplastic Anemia
Symptoms may develop gradually or appear suddenly. Common signs include:
- Persistent fatigue and weakness
- Pale or yellowish skin
- Shortness of breath
- Dizziness or lightheadedness
- Frequent infections
- Easy bruising or prolonged bleeding
Diagnosis of Hypoplastic Anemia
Proper diagnosis involves several steps, including:
1. Medical History and Physical Examination
Doctors assess symptoms, exposure history, and possible genetic conditions.
2. Blood Tests
- Complete Blood Count (CBC): Identifies reduced red blood cell, white blood cell, and platelet counts.
- Reticulocyte Count: Determines bone marrow’s ability to produce red blood cells.
3. Bone Marrow Biopsy
A biopsy confirms decreased cellular activity in bone marrow, a hallmark of hypoplastic anemia.
4. Additional Tests
- Viral infection screening
- Autoimmune antibody testing
- Genetic analysis for inherited conditions
Treatment Options for Hypoplastic Anemia
Treatment varies depending on the underlying cause and severity of the condition. Common approaches include:
1. Medications
- Immunosuppressants: Drugs such as cyclosporine and anti-thymocyte globulin (ATG) suppress immune responses that harm bone marrow.
- Growth Factors: Erythropoietin (EPO) and granulocyte colony-stimulating factor (G-CSF) stimulate blood cell production.
2. Blood Transfusions
Red blood cell or platelet transfusions manage symptoms and improve overall well-being.
3. Bone Marrow or Stem Cell Transplantation
This curative option replaces damaged bone marrow with healthy donor cells.
4. Lifestyle Management
- Avoiding environmental toxins
- Maintaining a balanced diet rich in iron, folate, and vitamin B12
- Regular medical checkups to monitor progress
Prognosis and Outlook
The prognosis for hypoplastic anemia depends on early diagnosis and appropriate treatment. With timely interventions such as immunotherapy, blood transfusions, or bone marrow transplants, many patients achieve stable blood counts and improved quality of life.
Prevention Strategies
While some causes are unavoidable, certain steps may reduce the risk:
- Limiting exposure to toxic chemicals
- Ensuring proper vaccination to prevent viral infections
- Genetic counseling for those with a family history of bone marrow disorders
Frequently Asked Questions
1. What is the primary cause of hypoplastic anemia?
Hypoplastic anemia can be caused by genetic conditions, chemical exposure, medications, or autoimmune disorders.
2. Can hypoplastic anemia be cured?
In some cases, a bone marrow transplant offers a complete cure. For others, treatment aims to manage symptoms effectively.
3. What lifestyle changes help manage hypoplastic anemia?
Avoiding toxins, maintaining a nutrient-rich diet, and adhering to medical advice can help manage the condition.
4. Is hypoplastic anemia the same as aplastic anemia?
While both involve bone marrow failure, hypoplastic anemia specifically refers to reduced bone marrow activity, while aplastic anemia is marked by complete marrow shutdown.
5. What is the survival rate for hypoplastic anemia patients?
Survival rates vary based on treatment response, with bone marrow transplants offering improved long-term outcomes in severe cases.