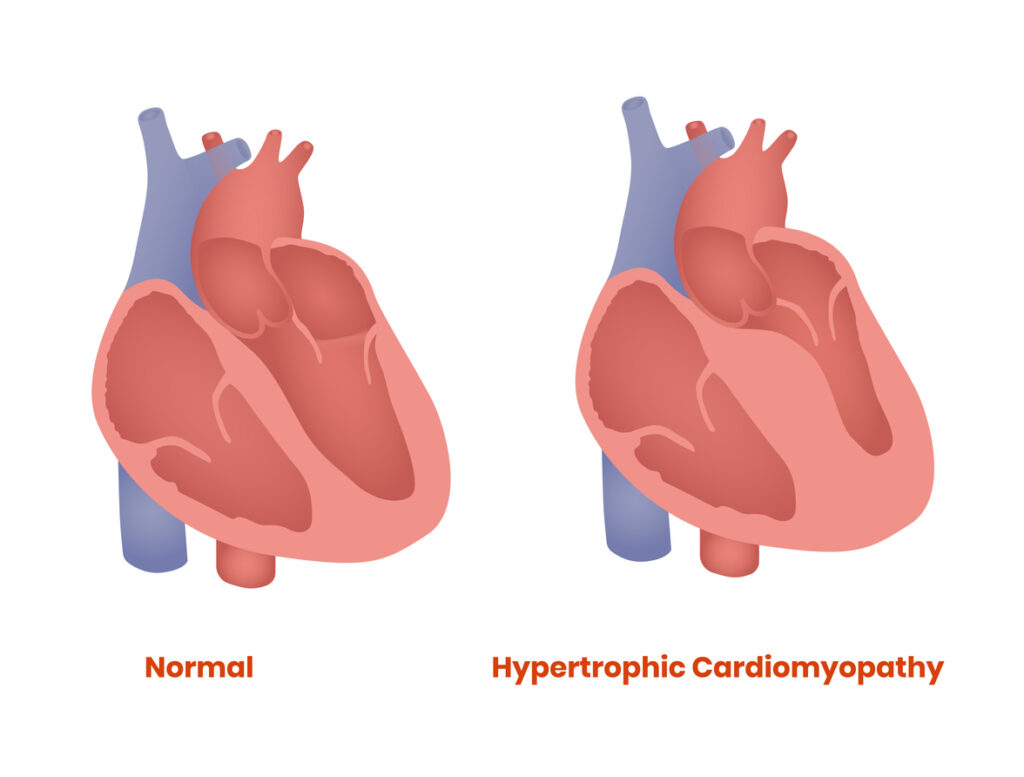
Hypertrophic Obstructive Cardiomyopathy (HOCM) is a complex and potentially life-threatening condition characterized by abnormal thickening of the heart muscle. This thickening often results in obstruction of blood flow from the heart, posing significant risks to patients if left untreated.
Causes and Risk Factors
HOCM is primarily a genetic disorder caused by mutations in the genes that encode cardiac muscle proteins. These mutations result in excessive growth of the heart muscle, particularly in the septum separating the left and right ventricles. Key risk factors include:
- Family history of cardiomyopathy or sudden cardiac death
- Genetic mutations related to sarcomere proteins
- Age (symptoms often emerge in adolescence or adulthood)
- Physical exertion in individuals with undiagnosed HOCM
Symptoms of Hypertrophic Obstructive Cardiomyopathy
The symptoms of HOCM can vary widely, ranging from mild to severe. Common signs include:
- Chest pain (angina)
- Shortness of breath, especially during exertion
- Palpitations or irregular heartbeats
- Dizziness or fainting spells
- Fatigue and reduced exercise capacity
In some cases, patients may remain asymptomatic, increasing the risk of sudden cardiac arrest.
Diagnosis and Screening
Accurate diagnosis is crucial for managing HOCM. Diagnostic tools include:
- Echocardiogram: Visualizes heart structure and identifies wall thickening.
- Electrocardiogram (ECG): Detects abnormal electrical activity.
- Cardiac MRI: Provides detailed imaging to assess muscle thickness and fibrosis.
- Genetic Testing: Identifies mutations associated with HOCM in families.
Pathophysiology of HOCM
In HOCM, the thickened septal wall obstructs blood flow from the left ventricle to the aorta. This obstruction increases pressure within the heart, leading to inefficient pumping and potential heart failure.
Treatment Options for HOCM
Treatment strategies for HOCM focus on symptom management and reducing the risk of complications.
Medications
- Beta-blockers: Reduce heart rate and improve blood flow.
- Calcium channel blockers: Relax heart muscles to enhance efficiency.
- Anti-arrhythmic drugs: Control abnormal heart rhythms.
Surgical Interventions
- Septal Myectomy: Surgical removal of thickened heart muscle.
- Alcohol Septal Ablation: A catheter-based procedure that reduces the thickened septum by injecting alcohol into targeted arteries.
Implantable Devices
- Implantable Cardioverter Defibrillator (ICD): Recommended for patients at risk of sudden cardiac arrest.
Lifestyle and Management
Effective lifestyle adjustments are critical for individuals with HOCM:
- Exercise moderation: Avoiding strenuous activities that may trigger symptoms.
- Medication adherence: Regular intake of prescribed drugs to manage symptoms.
- Routine monitoring: Frequent checkups to assess heart function and adjust treatments.
Prognosis and Long-Term Outlook
With proper diagnosis and management, most individuals with HOCM can lead fulfilling lives. Advances in treatment strategies continue to improve outcomes, reducing risks of heart failure and sudden cardiac events.
FAQs
1. What is the life expectancy of someone with HOCM?
With effective treatment, individuals can have a near-normal life expectancy. Early diagnosis and proper management are key.
2. Can HOCM be cured?
HOCM is a chronic condition but can be managed effectively with medications, lifestyle changes, and surgical options if needed.
3. Is HOCM hereditary?
Yes, HOCM is often inherited in an autosomal dominant pattern, meaning family members may be at risk.
4. What exercise is safe for people with HOCM?
Low-intensity activities such as walking and swimming are generally safe. Strenuous exercise should be avoided unless advised by a cardiologist.
5. How common is sudden cardiac death in HOCM patients?
Sudden cardiac death is a rare but serious risk in undiagnosed or poorly managed HOCM cases. ICDs may be recommended to reduce this risk.
Hypertrophic Obstructive Cardiomyopathy is a serious but manageable condition with proper diagnosis, medication, and lifestyle adjustments. Understanding symptoms, seeking timely treatment, and adopting preventive measures are vital for improving patient outcomes.