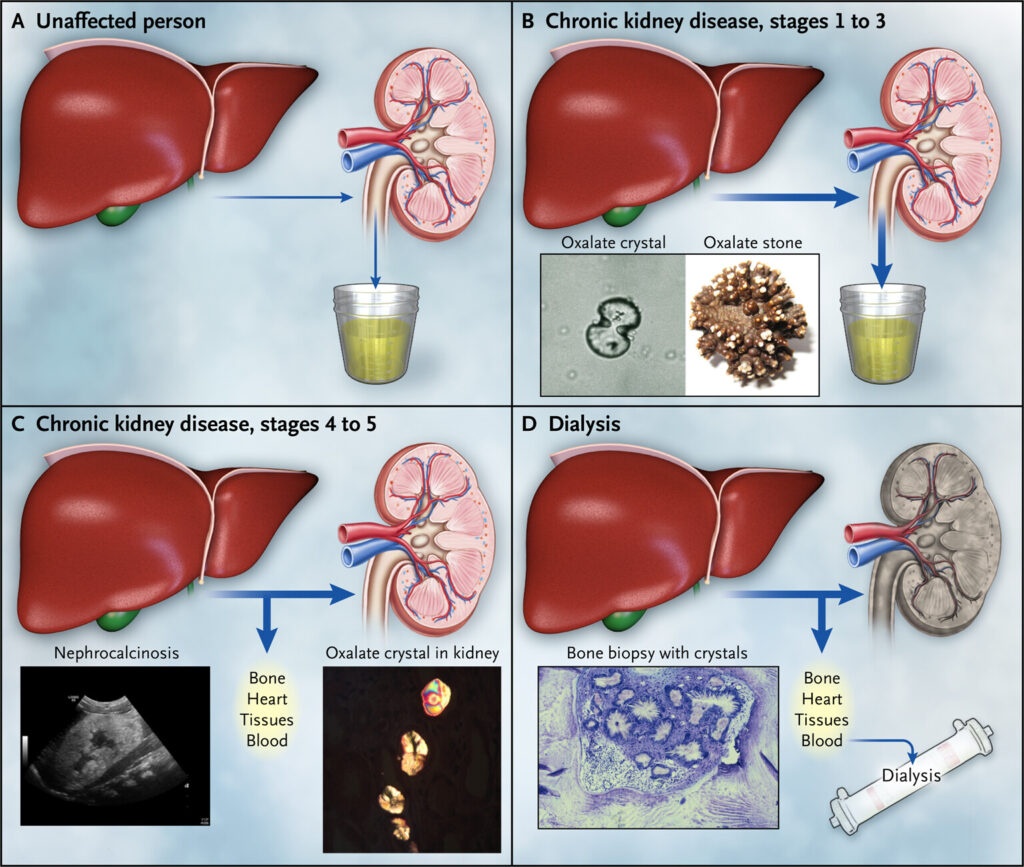
Hyperoxaluria is a medical condition characterized by excessive oxalate excretion in the urine. Oxalate is a natural compound found in certain foods and is also produced by the liver. When oxalate combines with calcium, it can form kidney stones and lead to severe renal complications if untreated.
Types
There are three primary types of hyperoxaluria, each with distinct causes and characteristics:
1. Primary Hyperoxaluria (PH)
- Genetic disorder: Caused by mutations in specific genes (AGXT, GRHPR, or HOGA1) that affect oxalate metabolism.
- Subtypes: PH1, PH2, and PH3, each linked to different genetic defects.
- Progression: Can lead to end-stage kidney disease if unmanaged.
2. Secondary Hyperoxaluria
- Diet-related: Excessive consumption of oxalate-rich foods such as spinach, nuts, and chocolate.
- Gastrointestinal disorders: Conditions like Crohn’s disease, short bowel syndrome, or bariatric surgery may increase oxalate absorption.
3. Idiopathic Hyperoxaluria
- Unknown cause: Often identified through urine tests without a clear dietary or genetic factor.
Causes
it may result from:
- Genetic mutations affecting oxalate metabolism
- Excessive dietary oxalate intake
- Intestinal conditions that boost oxalate absorption
- Vitamin B6 deficiency, impairing enzyme function
Symptoms
Symptoms often vary depending on the severity and type of hyperoxaluria. Common signs include:
- Severe and recurrent kidney stones
- Blood in the urine (hematuria)
- Frequent urinary tract infections (UTIs)
- Pain in the back or side
- Reduced kidney function leading to chronic kidney disease (CKD)
Diagnosis
Healthcare providers employ various diagnostic methods to confirm it:
- 24-hour urine test to measure oxalate levels
- Blood tests to assess kidney function
- Genetic testing for primary hyperoxaluria
- Imaging tests like ultrasound or CT scans to identify kidney stones
Treatments
Treatment strategies vary based on the type and severity of hyperoxaluria:
1. Dietary Management
- Reduce oxalate-rich foods like rhubarb, spinach, and almonds.
- Increase calcium intake to bind oxalates in the gut.
- Stay hydrated to dilute oxalate concentration in the urine.
2. Medications
- Potassium citrate to reduce stone formation
- Vitamin B6 supplements to lower oxalate production
- Probiotics such as Oxalobacter formigenes to aid oxalate breakdown
3. Surgical Interventions
- For severe cases involving large stones or kidney damage, surgical procedures like nephrolithotomy or kidney transplantation may be necessary.
Preventive Measures
To reduce the risk of hyperoxaluria:
- Maintain a balanced diet with controlled oxalate intake
- Drink plenty of fluids to support kidney function
- Monitor and manage gastrointestinal conditions
- Follow healthcare guidance on calcium and vitamin B6 supplementation
Complications
If untreated, hyperoxaluria may result in:
- Chronic kidney disease (CKD)
- Kidney failure requiring dialysis or transplantation
- Systemic oxalosis, where oxalate crystals accumulate in bones, joints, and other tissues
Hyperoxaluria is a complex yet manageable condition when diagnosed early and treated appropriately. With proper lifestyle adjustments, medication, and medical intervention, patients can significantly reduce the risk of severe kidney damage.
FAQs
What foods should be avoided in it?
Foods high in oxalates, such as spinach, beets, chocolate, and nuts, should be minimized.
Can it be cured?
While secondary hyperoxaluria can often be managed through dietary changes, primary hyperoxaluria may require lifelong treatment.
Is it hereditary?
Primary hyperoxaluria is a genetic disorder that can be inherited.
How is it diagnosed?
Diagnosis typically involves urine tests, blood work, and imaging studies, with genetic testing confirming primary hyperoxaluria.
What role does hydration play in managing?
Adequate hydration helps dilute urine oxalate levels, reducing the risk of kidney stone formation.