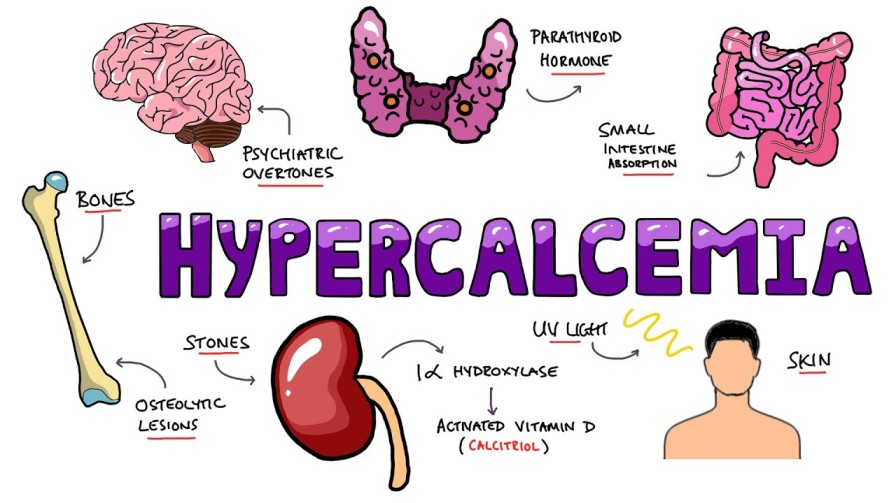
Hypercalcemia refers to an elevated calcium level in the blood above the normal range. Calcium is vital for bone health, muscle function, nerve transmission, and hormone release. However, excess calcium can pose serious health risks.
Causes of Hypercalcemia
Primary Hyperparathyroidism
- Overactive parathyroid glands produce excessive parathyroid hormone (PTH), leading to calcium release from bones and increased absorption in the intestines and kidneys.
Cancer-Related Hypercalcemia
- Certain cancers, particularly lung, breast, and multiple myeloma, can elevate calcium levels by releasing calcium from bones or producing hormone-like substances that mimic PTH.
Medications
- Drugs such as lithium, thiazide diuretics, and excessive vitamin D or calcium supplements may contribute to hypercalcemia.
Other Conditions
- Dehydration reduces blood volume, increasing calcium concentration.
- Immobility causes bone calcium release over time.
- Granulomatous Diseases like sarcoidosis can increase vitamin D production, enhancing calcium absorption.
Symptoms of Hypercalcemia
Mild cases may be asymptomatic, while severe cases can present with:
- Neurological Issues: Confusion, lethargy, fatigue, and memory problems
- Gastrointestinal Symptoms: Nausea, vomiting, constipation, and abdominal pain
- Renal Problems: Frequent urination, kidney stones, and dehydration
- Cardiac Symptoms: Arrhythmias, palpitations, and hypertension
Diagnosis of Hypercalcemia
Blood Tests
- Total Serum Calcium: Elevated calcium levels confirm hypercalcemia.
- Ionized Calcium: Measures biologically active calcium.
- Parathyroid Hormone (PTH) Test: Determines if the condition is linked to hyperparathyroidism.
Imaging Tests
- X-rays and CT Scans: Identify bone loss, fractures, or calcium deposits.
- Ultrasound or MRI: Helps detect parathyroid abnormalities or tumors.
Urine Tests
- Measures calcium excretion to assess kidney function and calcium balance.
Treatment for Hypercalcemia
Mild Hypercalcemia
- Hydration: Encourages calcium excretion through increased urine production.
- Dietary Changes: Reducing calcium intake and avoiding supplements can help.
Moderate to Severe Hypercalcemia
- Intravenous (IV) Fluids: Restores hydration and enhances calcium elimination.
- Bisphosphonates: Drugs like pamidronate and zoledronic acid inhibit bone calcium release.
- Calcitonin: Lowers calcium by blocking bone resorption.
- Corticosteroids: Useful in cases linked to granulomatous diseases.
- Dialysis: Necessary for severe cases where other treatments fail.
Complications of Hypercalcemia
Untreated hypercalcemia may lead to:
- Osteoporosis and fractures
- Kidney stones and renal failure
- Neurological complications, including coma
Preventing Hypercalcemia
- Maintain adequate hydration.
- Monitor calcium and vitamin D intake carefully.
- Regular medical checkups are crucial for individuals with conditions that increase hypercalcemia risk.
FAQs:
Q1: What is the most common cause of hypercalcemia?
A1: Primary hyperparathyroidism and malignancies are the leading causes of hypercalcemia.
Q2: Can dehydration cause hypercalcemia?
A2: Yes, dehydration reduces blood volume, thereby increasing calcium concentration.
Q3: What foods should be avoided in hypercalcemia?
A3: Foods high in calcium, such as dairy products, fortified cereals, and certain leafy greens, should be limited.
Q4: Is hypercalcemia a medical emergency?
A4: Severe hypercalcemia can be life-threatening and requires urgent medical attention.
Q5: Can hypercalcemia be prevented?
A5: Regular monitoring of calcium intake, hydration, and routine checkups can help prevent hypercalcemia.
Hypercalcemia is a serious condition that demands prompt diagnosis and management. Understanding its causes, symptoms, and treatments can help prevent severe complications. Individuals at risk should seek medical advice for regular screening and appropriate care.