Hyperbilirubinemia in newborns caused by hemolytic disease is a serious condition that requires prompt diagnosis and management. Hemolytic disease of the newborn (HDN) is characterized by the destruction of red blood cells due to maternal-fetal blood incompatibility. This leads to excessive bilirubin production, potentially resulting in severe complications like kernicterus.
Causes of Hyperbilirubinemia in Newborns
- Rh Incompatibility: Occurs when an Rh-negative mother carries an Rh-positive fetus, triggering maternal antibody production against fetal red cells.
- ABO Incompatibility: Arises when a mother with blood type O has a baby with type A or B, leading to hemolysis.
- G6PD Deficiency: This genetic disorder causes red blood cells to break down under oxidative stress.
- Other Blood Group Incompatibilities: Rare incompatibilities like Kell, Duffy, or Kidd antigen mismatches may contribute.
Pathophysiology of Hyperbilirubinemia in HDN
The immune-mediated destruction of fetal red blood cells results in the release of large amounts of hemoglobin. This hemoglobin is metabolized into bilirubin, overwhelming the newborn’s immature liver, which is unable to process the excess effectively.
Symptoms of Hyperbilirubinemia
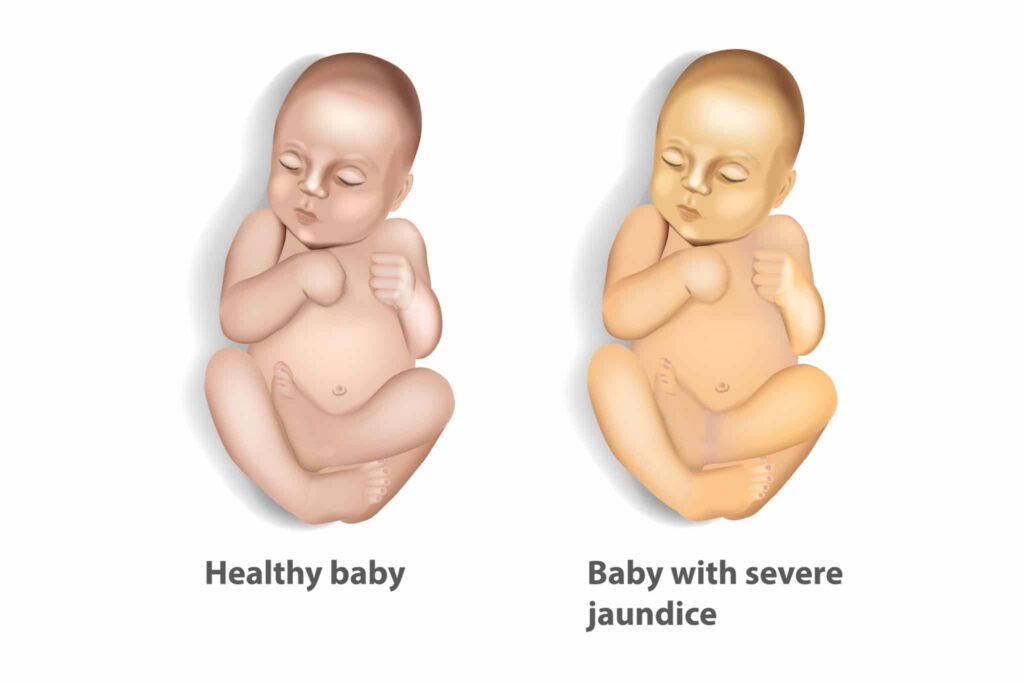
- Yellowing of skin and eyes (jaundice)
- Poor feeding and lethargy
- High-pitched crying
- Hypotonia or muscle weakness
- Seizures in severe cases
Diagnosis of Hyperbilirubinemia
- Clinical Examination: Observing jaundice levels in the skin, starting from the face and progressing downward.
- Bilirubin Levels: Total serum bilirubin (TSB) levels are measured to determine the severity.
- Coombs Test: Identifies antibodies attached to red blood cells in suspected cases of Rh or ABO incompatibility.
- Blood Smear Analysis: Reveals signs of hemolysis like schistocytes or spherocytes.
- Reticulocyte Count: Elevated in hemolytic processes.
Treatment Strategies
- Phototherapy: Utilizes blue light to convert bilirubin into a water-soluble form that can be excreted.
- Exchange Transfusion: Indicated in severe cases to rapidly lower bilirubin levels and remove sensitized red cells.
- Intravenous Immunoglobulin (IVIG): Administered to reduce hemolysis in cases of Rh and ABO incompatibility.
- Medications: Phenobarbital may enhance liver enzyme activity to promote bilirubin breakdown.
- Hydration and Feeding: Adequate nutrition helps reduce bilirubin levels by enhancing excretion.
Prevention of HDN-Associated Hyperbilirubinemia
- Prenatal Screening: Routine Rh and ABO typing to assess incompatibility risks.
- Rho(D) Immune Globulin (RhoGAM): Administered to Rh-negative mothers during pregnancy and postpartum to prevent antibody formation.
- Close Monitoring: Bilirubin levels should be closely observed in high-risk newborns for early intervention.
Complications of Untreated Hyperbilirubinemia
- Kernicterus: A severe form of brain damage resulting from excessive bilirubin crossing the blood-brain barrier.
- Permanent Neurological Damage: Including hearing loss, cerebral palsy, and developmental delays.
Prognosis and Long-Term Care
With timely diagnosis and treatment, most newborns recover fully without lasting effects. However, infants who develop kernicterus may require long-term therapy, including physical and speech therapy, to manage neurological impairments.
Hyperbilirubinemia due to hemolytic disease of the newborn is a preventable and treatable condition if identified early. Effective management strategies, including phototherapy and exchange transfusion, are essential to prevent severe complications. Prenatal care plays a crucial role in mitigating risks and ensuring positive outcomes for at-risk infants.