Hyperammonemia due to propionic acidemia (PA) is a severe metabolic condition resulting from the accumulation of ammonia in the bloodstream. Propionic acidemia is a rare autosomal recessive disorder that significantly impacts metabolic pathways, often leading to life-threatening complications if untreated. Understanding the underlying mechanisms, clinical presentation, and effective management strategies is crucial for improving patient outcomes.
What is Propionic Acidemia?
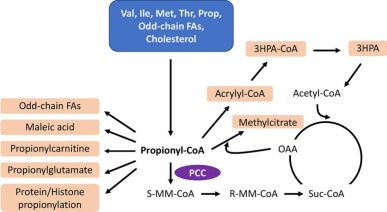
Propionic acidemia is a rare genetic disorder caused by mutations in the PCCA or PCCB genes, which encode for the propionyl-CoA carboxylase enzyme. This enzyme is essential for breaking down certain amino acids and lipids. In PA, the enzyme’s deficiency leads to an accumulation of propionyl-CoA and other toxic metabolites, ultimately causing hyperammonemia.
How Does Propionic Acidemia Cause Hyperammonemia?
The metabolic disruption in PA hinders the urea cycle, a critical process responsible for ammonia detoxification. The build-up of propionyl-CoA and other byproducts inhibits N-acetylglutamate synthase (NAGS), a key activator of carbamoyl phosphate synthetase I (CPS1) in the urea cycle. As a result, ammonia accumulates in the blood, leading to hyperammonemia.
Symptoms of Hyperammonemia in Propionic Acidemia
Patients with hyperammonemia due to PA may experience:
- Lethargy and poor feeding
- Vomiting
- Hypotonia (reduced muscle tone)
- Respiratory distress
- Seizures
- Coma in severe cases
Diagnostic Methods
Diagnosing hyperammonemia due to PA requires a combination of laboratory tests and genetic screening. Key diagnostic markers include:
- Elevated ammonia levels in blood tests
- Increased propionylcarnitine (C3) in plasma
- Urinary organic acid analysis revealing elevated methylcitrate and 3-hydroxypropionate
- Genetic testing for PCCA or PCCB mutations
Treatment Strategies
Managing hyperammonemia in PA requires immediate medical intervention to reduce ammonia levels and stabilize metabolic pathways. Treatment options include:
1. Acute Management
- Intravenous Ammonia Scavengers: Sodium benzoate and sodium phenylbutyrate facilitate ammonia excretion.
- Hemodialysis or Peritoneal Dialysis: Rapidly clears excess ammonia during life-threatening episodes.
- Intravenous Glucose and Lipid Infusions: Provide alternative energy sources to halt catabolism.
2. Long-Term Management
- Dietary Restrictions: Limiting protein intake while ensuring sufficient caloric supply.
- Carnitine Supplementation: Enhances mitochondrial function and facilitates propionyl-CoA elimination.
- Antibiotics: Reduces gut bacteria that produce propionate.
- Liver Transplantation: Recommended in severe or recurrent cases to improve metabolic stability.
Complications of Untreated Hyperammonemia in PA
If hyperammonemia is not addressed promptly, patients risk developing severe neurological impairment, developmental delays, and even fatal metabolic crises. Early diagnosis and aggressive treatment are crucial for improved outcomes.
Prognosis
The prognosis for individuals with PA varies significantly based on early diagnosis, effective management, and the frequency of metabolic crises. With proactive treatment strategies, many patients can achieve improved quality of life.
Preventive Measures
- Newborn Screening: Early detection through neonatal screening programs enables prompt intervention.
- Genetic Counseling: Recommended for at-risk families to understand the inheritance pattern and risk factors.
FAQs
Q1: What triggers hyperammonemia in PA patients?
A1: Triggers include illness, fasting, excessive protein intake, and metabolic stress.
Q2: Can hyperammonemia in PA be prevented?
A2: Proactive dietary management, regular medical monitoring, and effective treatment plans significantly reduce the risk.
Q3: What is the role of liver transplantation in PA management?
A3: Liver transplantation may improve metabolic stability and reduce ammonia buildup in severe cases.
Q4: Is genetic counseling necessary for PA?
A4: Yes, genetic counseling is crucial for families with a history of PA to understand inheritance risks and preventive care options.
Q5: Are ammonia-lowering medications safe for long-term use?
A5: When used under medical supervision, these medications are generally safe and effective for long-term ammonia control.
Hyperammonemia due to propionic acidemia requires vigilant management and early intervention to prevent severe complications. By combining prompt diagnosis, effective treatment strategies, and preventive measures, patients with PA can achieve improved long-term outcomes.

