Histiocytic neoplasms are a rare and heterogeneous group of disorders characterized by the proliferation of histiocytes, which are immune cells derived from the monocyte-macrophage lineage. These neoplasms encompass a spectrum of diseases with varying clinical presentations, prognoses, and therapeutic approaches. Understanding their classification, molecular underpinnings, and clinical manifestations is crucial for accurate diagnosis and management.
Classification of Histiocytic Neoplasms
The classification of histiocytic neoplasms has evolved with advancements in molecular diagnostics and a deeper understanding of their pathogenesis. According to the 5th edition of the World Health Organization (WHO) Classification of Haematolymphoid Tumours, histiocytic neoplasms are categorized into three main groups:
- Plasmacytoid Dendritic Cell Neoplasms: This group includes both mature forms associated with myeloid neoplasms and blastic variants.
- Langerhans Cells and Other Dendritic Cell Neoplasms: This category encompasses Langerhans cell histiocytosis (LCH) and related sarcomas, as well as indeterminate and interdigitated cell tumors.
- Histiocytic Neoplasms: This group includes:
- Juvenile Xanthogranuloma (JXG): A benign disorder typically presenting as skin nodules in children.
- Erdheim-Chester Disease (ECD): A systemic condition characterized by xanthomatous histiocyte infiltration, affecting multiple organs.
- Rosai-Dorfman Disease (RDD): Characterized by massive lymphadenopathy and histiocyte proliferation.
- ALK-Positive Histiocytosis: Defined by rearrangements involving the ALK gene.
- Histiocytic Sarcoma (HS): A malignant proliferation of histiocytes.
This classification reflects the diverse origins and behaviors of histiocytic neoplasms, aiding in precise diagnosis and treatment planning.
Epidemiology and Clinical Presentation
The epidemiology and clinical manifestations of histiocytic neoplasms vary significantly across different subtypes:
- Langerhans Cell Histiocytosis (LCH): Predominantly affects young children, especially males, with an incidence of 5–9 per million in those under 15 years. Commonly presents with bone lesions but can involve multiple organs, including the skin, liver, spleen, lungs, lymph nodes, central nervous system, and hematopoietic system.
- Erdheim-Chester Disease (ECD): Typically diagnosed in adults aged 55–60, with a male-to-female ratio of 3:1. Frequently involves the skeletal system (95% of cases), cardiovascular system, central nervous system, and retroperitoneum. Skin manifestations like xanthelasma are common.
- Juvenile Xanthogranuloma (JXG): Commonly presents in young boys as benign skin nodules that often resolve spontaneously. Extracutaneous or disseminated forms may require biopsy for accurate diagnosis.
- Rosai-Dorfman Disease (RDD): A rare disorder primarily affecting children and young adults, with a median onset age of 20 years and slight male predominance. Typically presents with massive bilateral cervical lymphadenopathy and constitutional symptoms such as fever and weight loss. Extranodal involvement occurs in 43% of cases, affecting the skin, soft tissue, upper respiratory tract, bones, eyes, and brain.
- Histiocytic Sarcoma (HS): A rare malignant neoplasm that can occur at any age, presenting with rapidly enlarging masses in lymph nodes or extranodal sites.
Molecular Pathogenesis
Advancements in genomic profiling have elucidated the molecular mechanisms driving histiocytic neoplasms:
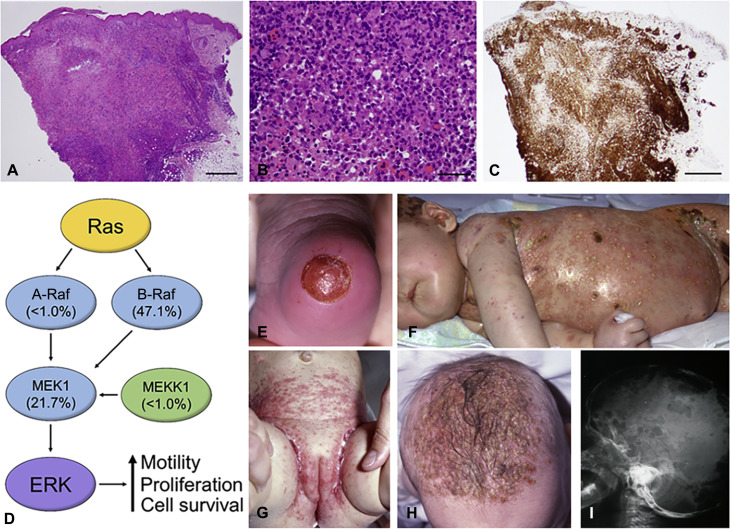
- MAPK Pathway Mutations: Approximately 50% of cases involve BRAF V600E mutations, leading to constitutive activation of the MAPK pathway. Other mutations in genes such as MAP2K1, ARAF, NRAS, and KRAS have been identified, particularly in BRAF wild-type cases.
- PI3K-AKT Pathway Alterations: Less commonly, mutations in the PI3K-AKT pathway contribute to disease pathogenesis.
Understanding these molecular alterations has significant implications for diagnosis, prognosis, and targeted therapy development.
Diagnostic Evaluation
Accurate diagnosis of histiocytic neoplasms involves a comprehensive approach:
- Histopathological Examination: Identifies characteristic histological features and immunophenotypes specific to each subtype. For instance, LCH cells express CD1a and langerin, while RDD cells are positive for S-100 protein.
- Imaging Studies: Assess the extent of organ involvement and guide biopsy sites.
- Molecular Testing: Next-generation sequencing (NGS) panels detect mutations in genes such as BRAF, MAP2K1, and others, aiding in diagnosis confirmation and therapeutic decision-making.