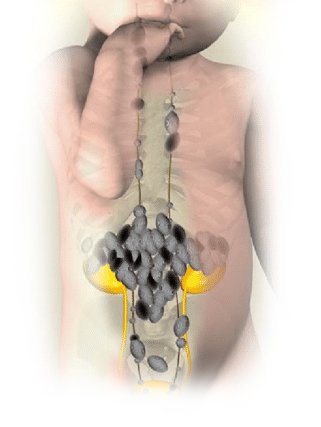
Neuroblastoma, a malignancy originating from neural crest cells, predominantly affects children under five years of age.
High-risk neuroblastoma, characterized by specific clinical and biological features, poses significant treatment challenges and is associated with poorer prognoses.
Risk Stratification and Prognostic Factors
Accurate risk assessment is crucial for tailoring treatment strategies. The International Neuroblastoma Risk Group Staging System (INRGSS) classifies tumors based on imaging-defined risk factors (IDRFs), patient age, histology, and genetic markers.
High-risk neuroblastoma is typically identified by:
- Age and Metastasis: Patients older than 18 months with metastatic disease often fall into the high-risk category.
- MYCN Amplification: Approximately 25% of neuroblastomas exhibit amplification of the MYCN oncogene, correlating with aggressive tumor behavior and poor outcomes.
- Segmental Chromosomal Aberrations (SCAs): Alterations such as deletions in chromosome arms 1p and 11q, and gains in 17q, are linked to adverse prognoses.
- ALK Mutations: Mutations in the anaplastic lymphoma kinase (ALK) gene occur in 5–10% of cases and are associated with unfavorable survival rates.
Treatment Modalities
Managing high-risk neuroblastoma necessitates an aggressive, multimodal approach:
Induction Therapy
Initial treatment comprises intensive chemotherapy aimed at reducing tumor burden and facilitating surgical resection.
Surgical Intervention
Post-chemotherapy, surgical removal of residual tumor mass is performed to achieve local disease control.
Consolidation with High-Dose Chemotherapy and Autologous Stem Cell Transplantation (HDCT/autoSCT)
High-dose chemotherapy followed by autologous stem cell rescue aims to eradicate minimal residual disease.
Tandem HDCT/autoSCT protocols have demonstrated improved event-free survival rates, reaching approximately 50–60%.
Radiotherapy
Targeted radiation therapy is employed to eliminate residual tumor cells, enhancing local control.
Immunotherapy
Post-consolidation, immunotherapeutic agents targeting disialoganglioside GD2 on neuroblastoma cells have shown promise in reducing relapse rates.
Advances in Targeted Therapies
Recent research has identified actionable genetic alterations in neuroblastoma, paving the way for targeted treatments:
ALK Inhibitors
The discovery of ALK gene mutations has led to the development of ALK inhibitors, offering potential therapeutic benefits for affected patients.
CAR T-Cell Therapy
Chimeric Antigen Receptor (CAR) T-cell therapy, a form of immunotherapy, has shown promise in treating neuroblastoma. Notably, a patient who underwent CAR T-cell therapy has remained in remission for 18 years, highlighting its potential efficacy.
Prognosis and Future Directions
Despite aggressive treatment, the five-year overall survival rate for high-risk neuroblastoma remains around 60%.
Ongoing research aims to improve outcomes through:
- Genetic Profiling: Understanding genetic predispositions can lead to personalized treatment approaches.
- Innovative Therapies: Incorporating novel agents and immunotherapies holds promise for enhancing survival rates.
- Clinical Trials: Participation in clinical trials offers access to cutting-edge treatments and contributes to advancing neuroblastoma care.
High-risk neuroblastoma presents significant therapeutic challenges. However, advancements in genetic understanding and treatment modalities offer hope for improved patient outcomes. A comprehensive, individualized approach remains essential in managing this complex pediatric malignancy.