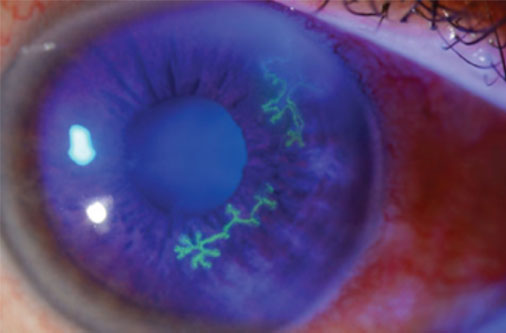
Herpes simplex dendritic keratitis is a common form of viral keratitis caused by the herpes simplex virus (HSV). This condition predominantly affects the cornea, leading to painful eye symptoms and potential vision impairment. Early diagnosis and appropriate treatment are essential to prevent complications.
What is Herpes Simplex Dendritic Keratitis?
Herpes simplex dendritic keratitis is an ocular infection that stems from the herpes simplex virus type 1 (HSV-1), though HSV-2 can also be a causative agent in rare cases. It is characterized by distinctive branching (dendritic) lesions on the corneal epithelium, which can cause discomfort and visual disturbances.
Causes and Risk Factors
The primary cause of herpes simplex dendritic keratitis is reactivation of latent HSV-1 in the trigeminal ganglion. Various triggers can initiate this reactivation, including:
- Stress
- Ultraviolet (UV) light exposure
- Trauma to the eye
- Use of corticosteroids
- Underlying immunosuppression
Symptoms of Herpes Simplex Dendritic Keratitis
Common symptoms include:
- Eye pain or discomfort
- Redness and irritation
- Blurred vision
- Tearing and discharge
- Photophobia (light sensitivity)
- Foreign body sensation in the eye
Diagnosis and Clinical Presentation
Diagnosis is typically based on clinical examination and patient history. Key diagnostic techniques include:
- Slit-lamp Examination: Reveals characteristic dendritic lesions with terminal bulbs.
- Fluorescein Staining: Highlights the branching dendritic ulcers.
- Polymerase Chain Reaction (PCR): Detects HSV DNA in corneal scrapings for definitive diagnosis.
- Viral Culture or Immunofluorescence: Used in complex or recurrent cases.
Treatment Options
Treatment for herpes simplex dendritic keratitis requires antiviral medications and supportive care. Recommended therapies include:
- Topical Antiviral Agents:
- Trifluridine 1% (every 2 hours)
- Ganciclovir ophthalmic gel 0.15% (5 times daily)
- Oral Antiviral Therapy:
- Acyclovir 400 mg (5 times daily)
- Valacyclovir 500 mg (twice daily)
- Debridement: Mechanical removal of infected corneal epithelium to reduce viral load.
- Corticosteroids: Reserved for stromal keratitis cases to reduce inflammation but require careful monitoring.
Prognosis and Complications
With early diagnosis and appropriate treatment, most patients experience favorable outcomes. However, complications may include:
- Corneal scarring
- Vision impairment
- Recurrence of infection
- Secondary bacterial infections
Prevention Strategies
Preventing herpes simplex dendritic keratitis involves managing risk factors and improving immune response:
- Use of UV-protective eyewear
- Stress management techniques
- Avoiding corticosteroid use without medical supervision
- Prophylactic antiviral medications in patients with frequent recurrences
Frequently Asked Questions:
Q1: Can herpes simplex dendritic keratitis cause blindness?
A: While rare, untreated or severe cases can result in corneal scarring and vision impairment, potentially leading to blindness.
Q2: Is herpes simplex dendritic keratitis contagious?
A: The virus itself is contagious, but keratitis symptoms are generally not transmitted directly between individuals.
Q3: How long does it take to recover from herpes simplex dendritic keratitis?
A: Most cases resolve within 2 to 3 weeks with appropriate antiviral treatment.
Q4: Can I wear contact lenses during treatment?
A: Contact lenses should be avoided during active infection to prevent worsening of the condition.
Q5: Is there a vaccine for herpes simplex virus?
A: Currently, there is no approved vaccine for HSV; however, antiviral medications effectively manage and reduce recurrence.
Herpes simplex dendritic keratitis is a serious ocular condition that requires prompt diagnosis and appropriate antiviral treatment. Understanding the causes, symptoms, and effective treatment strategies is crucial in preventing long-term vision damage and managing recurrence.