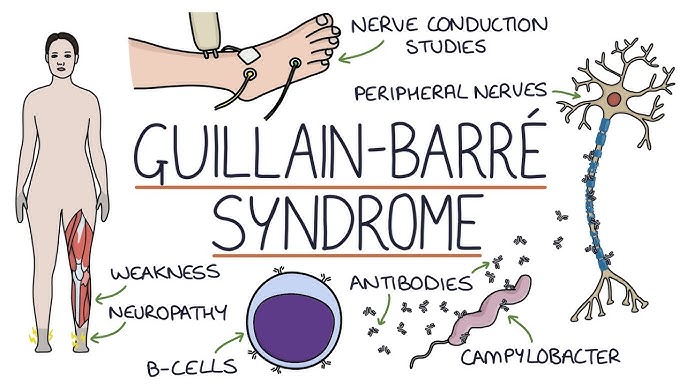
Guillain-Barré Syndrome (GBS) is a rare but serious autoimmune disorder in which the body’s immune system mistakenly attacks the peripheral nerves. This condition can lead to muscle weakness, numbness, and, in severe cases, paralysis. Early diagnosis and prompt treatment are crucial for managing symptoms and improving recovery outcomes.
What Causes Guillain-Barré Syndrome?
GBS typically develops after a viral or bacterial infection. Common triggers include:
- Respiratory infections
- Gastrointestinal infections (e.g., Campylobacter jejuni)
- Influenza virus
- Cytomegalovirus (CMV)
- Epstein-Barr virus (EBV)
- Zika virus
- COVID-19 infection or vaccination (rare cases)
Symptoms of Guillain-Barré Syndrome
GBS symptoms often develop rapidly and may include:
- Tingling sensations in the hands and feet
- Muscle weakness starting in the legs and spreading upward
- Loss of reflexes
- Difficulty breathing in severe cases
- Heart rate irregularities
- Facial paralysis or vision issues
Types of Guillain-Barré Syndrome
GBS manifests in different forms, including:
- Acute Inflammatory Demyelinating Polyneuropathy (AIDP): The most common type in Western countries, causing muscle weakness that starts in the lower body.
- Miller Fisher Syndrome (MFS): Starts with eye paralysis and poor balance.
- Acute Motor Axonal Neuropathy (AMAN): More common in Asia and Latin America, causing severe muscle weakness.
- Acute Motor-Sensory Axonal Neuropathy (AMSAN): A more severe variant of AMAN, involving both motor and sensory nerves.
How Is Guillain-Barré Syndrome Diagnosed?
Medical professionals typically follow these steps to confirm a GBS diagnosis:
- Clinical evaluation: Assessing muscle weakness and reflex responses.
- Lumbar puncture (spinal tap): Identifying elevated protein levels in cerebrospinal fluid.
- Nerve conduction studies: Evaluating nerve signals.
- Electromyography (EMG): Measuring muscle response to nerve signals.
Treatment Options for Guillain-Barré Syndrome
GBS treatment aims to reduce immune system activity and manage symptoms. Key treatments include:
- Intravenous immunoglobulin (IVIG): Antibodies from donors to block harmful immune responses.
- Plasmapheresis (plasma exchange): Removing harmful antibodies from the blood.
- Pain management medications: Relieving nerve pain and discomfort.
- Physical therapy: Aiding recovery through muscle strengthening exercises.
Potential Complications of GBS
While most individuals recover, some may experience long-term effects, including:
- Chronic fatigue
- Persistent muscle weakness
- Pain or numbness
- Breathing issues requiring prolonged ventilation
Preventing Guillain-Barré Syndrome
While GBS cannot always be prevented, reducing risk factors may help:
- Maintain good hygiene to reduce infection risk.
- Stay updated on vaccinations to prevent viral infections.
- Seek prompt treatment for bacterial illnesses.
FAQs on Guillain-Barré Syndrome
1. Is Guillain-Barré Syndrome fatal?
- While rare, severe cases can be life-threatening if breathing muscles are impacted. Timely medical care is crucial.
2. Can GBS recur?
- Recurrence is rare but possible. Individuals with a history of GBS should remain vigilant about early symptoms.
3. How long does it take to recover from GBS?
- Recovery typically takes 6 months to 1 year, though some may experience residual effects for longer.
4. Can children develop GBS?
- Yes, while rare, GBS can affect children and requires immediate medical attention.
5. Are there any lifestyle changes to aid GBS recovery?
- A balanced diet, regular physical therapy, and mental well-being support can enhance recovery.
Guillain-Barré Syndrome is a rare but serious neurological condition requiring swift diagnosis and treatment. With proper medical care, most patients can achieve significant recovery. Awareness, early intervention, and comprehensive treatment are vital for optimal outcomes.