Haemophilus parainfluenzae is a facultatively anaerobic, gram-negative coccobacillus commonly found as part of the human respiratory tract microbiota. While typically a commensal organism, it may act as an opportunistic pathogen under specific conditions, particularly in individuals with compromised immune systems or chronic respiratory diseases.
Characteristics of Haemophilus parainfluenzae:
- Gram-negative, pleomorphic coccobacilli
- Facultative anaerobe
- Non-encapsulated
- Requires X (hemin) and V (NAD) factors for growth
Chronic Bronchitis: An Overview
Chronic bronchitis is defined as persistent inflammation of the bronchial tubes, resulting in mucus overproduction and a chronic cough that lasts for at least three months per year for two consecutive years. It is a key component of chronic obstructive pulmonary disease (COPD).
Common Symptoms of Chronic Bronchitis:
- Persistent productive cough
- Shortness of breath
- Wheezing
- Chest discomfort
- Fatigue
The Connection Between Haemophilus parainfluenzae and Chronic Bronchitis
Chronic bronchitis patients are susceptible to bacterial colonization due to impaired mucociliary clearance and inflamed airways. Haemophilus parainfluenzae is a leading bacterial pathogen isolated in chronic bronchitis exacerbations, contributing to airway damage and increased mucus production.
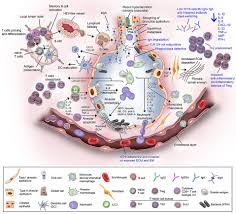
Pathogenesis:
- Colonization: Bacteria adhere to the respiratory epithelium.
- Evasion of Host Defenses: Resists immune clearance mechanisms.
- Inflammatory Response: Triggers cytokine production and neutrophilic inflammation.
- Tissue Damage: Causes epithelial disruption and airway remodeling.
Diagnosis of Haemophilus parainfluenzae Chronic Bronchitis
Accurate diagnosis involves clinical evaluation and laboratory confirmation. Key diagnostic approaches include:
- Clinical History and Examination: Assessment of chronic cough, sputum production, and respiratory distress.
- Sputum Culture and PCR Testing: Identification of Haemophilus parainfluenzae through microbiological culture or polymerase chain reaction (PCR).
- Pulmonary Function Tests: Evaluates airflow obstruction severity.
- Chest Imaging: Detects structural lung changes and excludes other pathologies.
Treatment Strategies for Haemophilus parainfluenzae-Associated Chronic Bronchitis
Treatment aims to eradicate bacterial infection, manage symptoms, and prevent exacerbations. Therapeutic approaches include:
1. Antibiotic Therapy
Effective antibiotics against Haemophilus parainfluenzae include:
- Aminopenicillins (e.g., amoxicillin-clavulanate)
- Cephalosporins (e.g., cefuroxime)
- Macrolides (e.g., azithromycin)
- Fluoroquinolones (e.g., levofloxacin)
2. Symptomatic Management
- Bronchodilators: Relieve airway constriction.
- Inhaled Corticosteroids: Reduce inflammation.
- Mucolytics: Facilitate mucus clearance.
3. Supportive Care
- Smoking Cessation: Critical to prevent disease progression.
- Pulmonary Rehabilitation: Improves lung function and quality of life.
Prevention and Long-Term Management
Preventive measures are essential to reduce the incidence and severity of Haemophilus parainfluenzae chronic bronchitis:
- Vaccination: Influenza and pneumococcal vaccines reduce respiratory infections.
- Hygiene Practices: Hand hygiene and respiratory precautions lower bacterial transmission.
- Environmental Modifications: Avoiding air pollutants and smoking cessation.
Follow-Up and Monitoring
Patients with chronic bronchitis require regular follow-up to monitor symptoms, lung function, and treatment efficacy.
Haemophilus parainfluenzae plays a significant role in the pathogenesis and exacerbation of chronic bronchitis. Prompt diagnosis and tailored antibiotic therapy, combined with supportive care, are vital for effective management. Preventive strategies and long-term monitoring can mitigate disease progression and improve patient outcomes.