Haemophilus parainfluenzae is a facultative anaerobic gram-negative bacterium commonly residing in the human upper respiratory tract. While generally part of the normal flora, it can become pathogenic under certain conditions, leading to respiratory infections such as bronchitis.
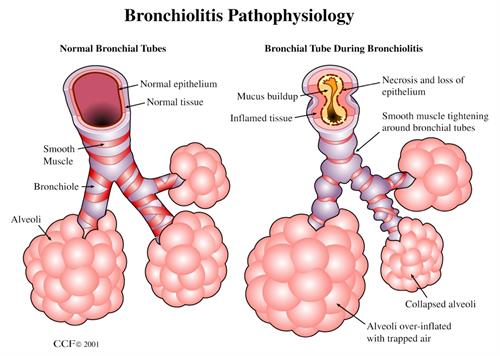
Bronchitis caused by Haemophilus parainfluenzae involves inflammation of the bronchial tubes, resulting in cough, mucus production, and breathing difficulties. This bacterium is an opportunistic pathogen, meaning it often causes disease in individuals with compromised immune systems or underlying lung conditions.
Causes and Risk Factors
Haemophilus parainfluenzae bronchitis typically arises due to bacterial overgrowth when the body’s natural defenses are weakened. Key risk factors include:
- Immunosuppression: Conditions like HIV/AIDS or chemotherapy weaken the immune system.
- Chronic Respiratory Diseases: Asthma, chronic obstructive pulmonary disease (COPD), and cystic fibrosis increase susceptibility.
- Smoking: Damages bronchial lining, promoting bacterial colonization.
- Viral Infections: Influenza or common cold can pave the way for secondary bacterial infections.
- Age Factors: Infants, the elderly, and immunocompromised individuals are at higher risk.
Symptoms of Haemophilus Parainfluenzae Bronchitis
The clinical presentation of Haemophilus parainfluenzae bronchitis is similar to other bacterial respiratory infections. Common symptoms include:
- Persistent cough with yellow or green sputum
- Wheezing and shortness of breath
- Chest discomfort and pain
- Fever and chills
- Fatigue and malaise
In severe cases, bronchitis can lead to complications such as pneumonia or sepsis if left untreated.
Diagnosis and Laboratory Testing
Accurate diagnosis is critical to distinguish Haemophilus parainfluenzae bronchitis from other causes of respiratory illness. Diagnostic steps include:
- Clinical Evaluation: Comprehensive medical history and physical examination.
- Sputum Culture: Identifies bacterial pathogens through culture and sensitivity testing.
- Polymerase Chain Reaction (PCR): Detects bacterial DNA for precise identification.
- Chest X-ray: Rules out pneumonia or other structural lung abnormalities.
- Blood Tests: Measures inflammation markers (C-reactive protein, white blood cell count).
Treatment of Haemophilus Parainfluenzae Bronchitis
Effective management involves targeted antimicrobial therapy and symptomatic relief. Treatment strategies include:
- Antibiotics:
- First-line: Beta-lactam antibiotics (amoxicillin-clavulanate)
- Alternative: Macrolides (azithromycin) or fluoroquinolones for resistant strains
- Supportive Care:
- Hydration to thin mucus secretions
- Bronchodilators for airway constriction
- Antipyretics (e.g., acetaminophen) for fever control
- Monitoring and Follow-Up:
- Regular assessment to prevent complications
- Repeat cultures if symptoms persist despite treatment
Prevention Strategies
Preventive measures reduce the risk of Haemophilus parainfluenzae bronchitis, especially in vulnerable populations. Recommendations include:
- Vaccination: Routine immunization against Haemophilus influenzae type B (Hib) indirectly protects against related species.
- Good Hygiene Practices: Frequent handwashing and respiratory etiquette.
- Avoid Smoking: Reduces bronchial damage and susceptibility to infection.
- Manage Chronic Conditions: Control asthma and COPD to minimize infection risk.
Complications and Prognosis
Untreated Haemophilus parainfluenzae bronchitis can progress to severe respiratory issues. Possible complications include:
- Pneumonia
- Respiratory failure
- Bacteremia and sepsis
With prompt diagnosis and appropriate antibiotic therapy, the prognosis is generally favorable. However, immunocompromised patients may experience a protracted course or recurrence.
Haemophilus parainfluenzae bronchitis is a significant cause of bacterial respiratory infection, especially in individuals with compromised immunity or chronic lung disease. Prompt recognition, accurate diagnosis, and targeted antibiotic therapy are essential to prevent complications and ensure favorable patient outcomes. Implementing preventive strategies is crucial to reducing the burden of this bacterial pathogen on public health.