Haemophilus parahaemolyticus is a facultative anaerobic Gram-negative bacterium known to cause a variety of human infections. Although rare, Haemophilus parahaemolyticus pneumonia is a serious respiratory condition requiring prompt diagnosis and treatment. This article provides a detailed overview of its etiology, clinical manifestations, diagnostic approaches, therapeutic options, and preventive measures.
What Is Haemophilus parahaemolyticus?
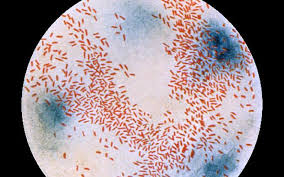
Haemophilus parahaemolyticus belongs to the Haemophilus genus, which comprises small, pleomorphic, and non-motile bacteria. While most infections caused by Haemophilus species are attributed to Haemophilus influenzae, Haemophilus parahaemolyticus is an emerging pathogen associated with respiratory tract infections.
Bacteriological Characteristics:
- Morphology: Small, Gram-negative coccobacilli
- Growth Requirements: Requires V factor (nicotinamide adenine dinucleotide)
- Oxygen Tolerance: Facultative anaerobe
- Transmission: Respiratory droplets, direct contact with respiratory secretions
Pathogenesis of Haemophilus parahaemolyticus Pneumonia
Infection typically occurs through inhalation of aerosolized bacteria. The bacterium adheres to and invades respiratory epithelial cells, causing localized inflammation and subsequent lung tissue damage. Immunocompromised individuals, older adults, and those with chronic respiratory conditions are at heightened risk.
Clinical Manifestations
Symptoms of Haemophilus parahaemolyticus pneumonia often resemble other bacterial pneumonias but may present more acutely in vulnerable populations.
Common Symptoms:
- Persistent cough with purulent sputum
- Dyspnea (shortness of breath)
- Chest pain, especially during breathing
- Fever and chills
- Fatigue and malaise
Severe Complications:
- Respiratory failure
- Pleural effusion
- Sepsis
Diagnosis of Haemophilus parahaemolyticus Pneumonia
Accurate and timely diagnosis is crucial for effective management. Several diagnostic modalities are utilized to confirm the presence of Haemophilus parahaemolyticus in pulmonary infections.
Diagnostic Methods:
- Clinical Assessment: Patient history and physical examination.
- Microbiological Testing:
- Sputum culture and Gram staining
- Blood culture in cases of systemic involvement
- Molecular Diagnostics: Polymerase chain reaction (PCR) for species-specific identification.
- Imaging Studies:
- Chest X-ray: Detects lung consolidation or infiltrates.
- Computed tomography (CT): Identifies localized abscesses or pleural effusion.
Treatment Strategies
Early initiation of targeted antimicrobial therapy is essential to mitigate disease progression and reduce mortality.
Antibiotic Therapy:
- First-line Treatment: Third-generation cephalosporins (e.g., ceftriaxone)
- Alternative Agents: Fluoroquinolones or amoxicillin-clavulanate for penicillin-sensitive cases
- Severe Infections: Combination therapy with broad-spectrum antibiotics pending culture results
Supportive Care:
- Oxygen supplementation for hypoxia
- Intravenous fluids to maintain hemodynamic stability
- Mechanical ventilation in severe respiratory failure
Prevention and Control Measures
Reducing the risk of Haemophilus parahaemolyticus pneumonia involves both individual and public health interventions.
Preventive Strategies:
- Vaccination: Although no specific vaccine exists for Haemophilus parahaemolyticus, Haemophilus influenzae type b (Hib) vaccine may reduce related infections.
- Infection Control: Hand hygiene, respiratory etiquette, and disinfection of shared spaces.
- Risk Reduction: Managing chronic conditions and avoiding exposure in healthcare settings.
Prognosis
With prompt and appropriate antibiotic therapy, the prognosis is generally favorable. However, delays in diagnosis and treatment can lead to severe complications and increased mortality.
Factors Influencing Prognosis:
- Timeliness of treatment initiation
- Patient comorbidities
- Pathogen antimicrobial resistance
Haemophilus parahaemolyticus pneumonia, while uncommon, poses a significant threat to vulnerable populations. Early recognition, precise diagnosis, and targeted antimicrobial therapy are pivotal in managing and preventing adverse outcomes. Enhanced awareness and adherence to preventive measures can mitigate the disease burden and improve patient outcomes.