Haemophilus osteomyelitis is a rare but serious bacterial infection that affects the bones. This condition is primarily caused by Haemophilus influenzae, particularly type b (Hib), though other Haemophilus species may also be implicated. It typically affects children under the age of five but can also present in adults, especially those with compromised immune systems. Prompt diagnosis and appropriate antibiotic therapy are crucial to prevent complications such as bone destruction, sepsis, and permanent disability.
Etiology and Pathogenesis of Haemophilus Osteomyelitis
Haemophilus osteomyelitis results from hematogenous spread, direct inoculation, or contiguous extension. In children, the infection commonly originates from bacteremia following respiratory tract infections. The metaphysis of long bones, rich in blood supply, is the most frequently affected site.
Pathophysiology of Haemophilus Osteomyelitis
- Bacterial Invasion: Entry of Haemophilus bacteria into the bloodstream via mucosal surfaces.
- Hematogenous Spread: Bacteria circulate and localize in the highly vascularized metaphyseal regions.
- Inflammation and Bone Destruction: Bacterial toxins induce inflammation, leading to bone necrosis and abscess formation.
Clinical Presentation of Haemophilus Osteomyelitis
Symptoms vary based on age, immune status, and the duration of infection. Common clinical signs include:
- Localized Bone Pain: Severe pain and tenderness at the affected site.
- Fever and Malaise: Systemic symptoms such as high fever and fatigue.
- Swelling and Erythema: Overlying skin may appear red, swollen, and warm.
- Limited Range of Motion: Joint involvement may restrict mobility.
- Irritability in Children: Especially in non-verbal pediatric patients.
Diagnostic Approach to Haemophilus Osteomyelitis
Early diagnosis is essential for optimal outcomes. Diagnostic methods include:
1. Clinical Evaluation
A thorough history and physical examination focusing on recent infections and localized symptoms.
2. Laboratory Investigations
- Complete Blood Count (CBC): Elevated white blood cells (WBCs) suggest infection.
- Inflammatory Markers: Increased C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR).
- Blood Cultures: Identification of Haemophilus species confirms bacteremia.
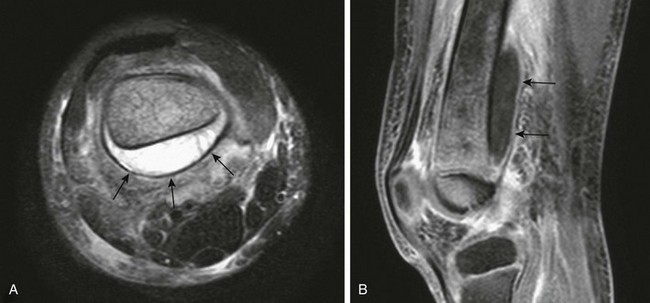
3. Imaging Studies
- X-ray: Detects late-stage bone destruction.
- MRI: Preferred for early detection and soft-tissue involvement.
- Bone Scan: Useful for localizing occult infections.
Treatment of Haemophilus Osteomyelitis
Early, aggressive intervention is vital. Treatment includes:
1. Antibiotic Therapy
- Empirical Therapy: Third-generation cephalosporins (e.g., ceftriaxone) until culture results.
- Targeted Therapy: Based on antibiotic susceptibility; typically 4-6 weeks of IV antibiotics followed by oral therapy.
2. Surgical Management
Indicated in cases of abscess formation or failure of medical therapy:
- Debridement: Removal of necrotic bone tissue.
- Drainage: Aspiration or surgical drainage of abscesses.
3. Supportive Care
- Pain Management: Non-steroidal anti-inflammatory drugs (NSAIDs) or analgesics.
- Physical Therapy: Restores function and prevents joint stiffness.
Prognosis and Complications
With early diagnosis and appropriate treatment, most patients recover fully. However, delayed or inadequate therapy may lead to:
- Chronic osteomyelitis
- Growth disturbances (in children)
- Pathological fractures
- Septic arthritis
Prevention of Haemophilus Osteomyelitis
- Vaccination: Hib vaccine significantly reduces the incidence.
- Prompt Infection Control: Timely treatment of respiratory and other bacterial infections.
- Aseptic Technique: During surgical and invasive procedures.
Haemophilus osteomyelitis is a potentially life-threatening condition requiring early recognition and prompt intervention. Advances in diagnostic methods, targeted antibiotic regimens, and preventive measures such as Hib vaccination have significantly improved outcomes. Awareness of clinical presentations, timely diagnosis, and comprehensive management are essential to prevent complications and ensure optimal patient recovery.